Superagers: Why resistant to age-related memory decline?
An observational study investigated whether age-related memory decline may not affect superagers, or those 80 years and older who possess the cognitive abilities of people who are decades younger.
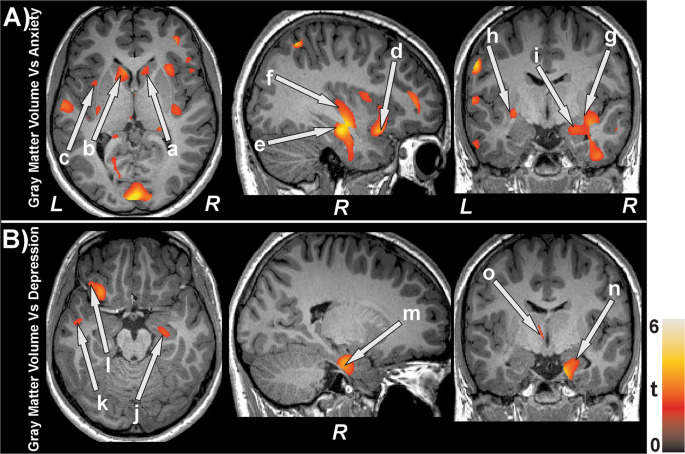
In comparison to older persons with cognitive deterioration, the octogenarians with strong memory retention moved more quickly and experienced lower levels of worry and depression. Additionally, MRI scans revealed that certain memory-related brain regions had increased grey matter in super-agers.
Superagers are people over the age of 80 whose recollections of their past are just as clear as those of others who are 20 or 30 years younger. Scientific research is becoming increasingly interested in the mechanisms of superaging.

According to a recent study, older persons with cognitive decline had higher rates of anxiety and despair compared to octogenarians with strong memory retention. They also do better on movement tests.
The researchers speculate that such superagers may also have more grey matter in their brains.
In a press release, the study’s first author Marta Garo-Pascual, a Ph.D. candidate at the Technical University of Madrid in Spain who studies healthy memory ageing, stated:
“We are now getting closer to answering one of the most important outstanding concerns about superchargers: whether they are actually resistant to age-related memory decline or whether they have coping mechanisms that allow them to outperform their contemporaries in overcoming this decline. Although the specific causes of super agers resistance to these processes are still unknown, our data suggest they do. We may be able to learn vital information about the mechanisms underlying the maintenance of memory function well into old life by investigating the connections between superaging and movement speed in more detail.”
Superagers: Exercise promotes the health of the brain
For the study, 55 typical older persons and 64 superagers who were identified by a memory test used in a prior study on Alzheimer’s disease were compared. The average age of research participants was 79.5 years or higher.
The Timed Up and Go Test, which assesses mobility, and a finger-tapping test, which gauges fine motor function, revealed that the superagers outperformed the general population.
Even when super agers reported no appreciable change in exercise levels from the older people in the control group, the findings persisted.
The study’s principal author, Dr. Bryan Strange, a neurologist at the Technical University of Denmark, noted that although superagers report similar activity levels to average older adults, it’s possible that they engage in more physically taxing hobbies like gardening or stair climbing.
“There are many direct and indirect benefits of being physically active that may contribute to improved cognitive abilities in old age, from lower blood pressure and obesity levels to increased blood flow to the brain,” stated Dr. Bryan Strange.
It’s also plausible that the reason superagers move more quickly is because their brains are in greater health to begin with, according to Strange.
The amount of grey matter in superagers brains is higher.
The results also supported earlier studies that found super-agers have more grey matter in the brain regions linked to memory.
Researchers Dr. Alexandra Touroutoglous, Dr. Bonnie Wong, and Dr. Joseph M Andreano of Harvard Medical School wrote in an editorial statement that accompanied the article that this discovery predominantly focused on the medial temporal lobe of the brain, “which is consistent with previous research.”
The comments pointed out that previous studies on the anterior mid-cingulate cortex, another crucial area of the brain, reported more cortical thickness and stronger functional connectivity among super-agers, who in turn had greater memory performance.
The attention, memory, executive function, and motivation are just a few of the processes that the anterior mid-cingulate cortex is involved in.
The researchers concluded that “[the] greater performance of super agers relative to typical older adults may not only reflect differences in motivation, executive function, and persistence in the face of difficulty, which suggests that super-agers have a higher level of tenacity than typical older adults.”
Compared to other older individuals, superagers age differently.
According to the University of Madrid study, there were no discernible differences between superagers and other adults of a similar age in terms of biomarkers or genetic risk factors for neurological illness. This suggests that another protective mechanism may be at play.
Similar levels of dementia blood biomarkers were found in both the superager and standard older adult groups, the researchers said, “suggesting that group differences reflect inherent superager resistance to typical age-related memory loss.”
The study’s large sample size, according to Dr. S. Jay Olshansky, a professor in the Division of Epidemiology and Biostatistics at the University of Illinois at Chicago School of Public Health, makes the results an essential addition to the field of “geroscience,” the research of mechanisms that cause aging.
Dr. Olshansky stated, “We do a lot of things to shorten our lives by adopting unhealthy lifestyles,” and many superchargers and centenarians people who live past 100 live longer and have better cognitive health because they age differently from the general population.
Do super-agers have a hereditary propensity for aging?
The appearance of some children of superchargers, Dr. Olshansky recalled, supported the idea that some people’s “biological time clock ticks at a slower rate” due to genetic factors. This is said to also explain why the superchargers in the Spanish study also performed better on movement tests.
Even though they have completed 80 orbits around the sun, he claimed that they are not biologically 80 years old.
“Asking superagers for their key to longevity is therefore ludicrous because they have no idea. They recently emerged as the birth genetic lottery winner.
The latest study, according to Dr. Olshansky, attempts to better understand why some people age differently than others and determine whether the process may be changed.
He said, “Start with not shortening your life,” in the meanwhile. “We will still age and pass away, even if you control all the risk factors,” he stated. We are at the mercy of our genes, but we have some power over those genes.
REFERENCES:
- https://pavilionhealthtoday.com/gm/super-agers-resistant-to-age-related-memory-decline/
- https://www.medicalnewstoday.com/articles/why-are-superagers-resistant-to-age-related-memory-decline
- https://www.medpagetoday.com/neurology/dementia/105495
For Mental disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_478