Boost skin cancer immunotherapy by targeting proteins.
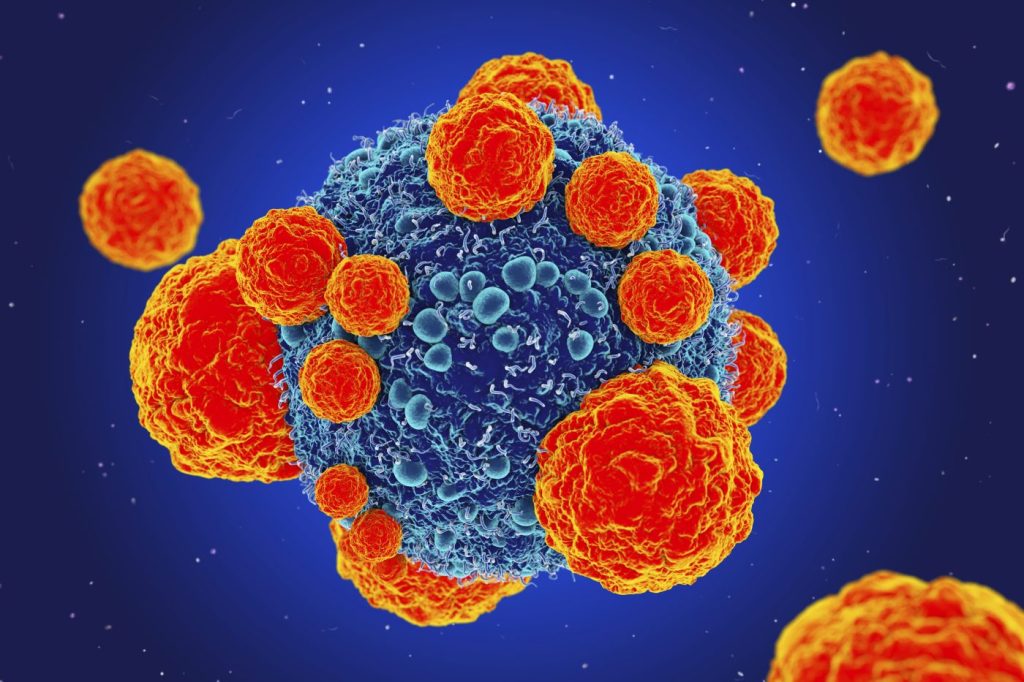
A protein that aids tumors in evading immune response and supports the growth of melanoma has been discovered by new research.
According to researchers, immunotherapy should be more effective with tailored medicines directed particularly at this protein.
One of the most prevalent malignancies, melanoma is typically brought on by exposure to UV light, while hereditary factors also play a part in its development.
Experts advise staying away from tanning beds and direct sunshine, as well as keeping an eye out for any moles that seem out of the ordinary.
The growth of melanoma has been the subject of recent research, which has also opened up new potential treatment options.
In a study that was published in the journal Science Advances, researchers showed how a protein called NR2F6 aids tumor growth by assisting tumours to elude the immune system.
The scientists discovered that in mice, eliminating the protein made the immune treatment work more effectively.
“This tells us that NR2F6 helps melanoma evade the immune system, and without it, the immune system can more readily suppress tumour growth,” said Dr. Hyungsoo Kim, a research assistant professor at Sanford Burnham Prebys, a research centre in La Jolla, California, and the study’s first author.
Treatments that prevent the protein’s action are thought to be twice as effective since it behaves the same way whether it is in a tumor or the tissues around it.
The scientists are currently searching for fresh medications that can particularly target NR2F6.
learning about melanoma
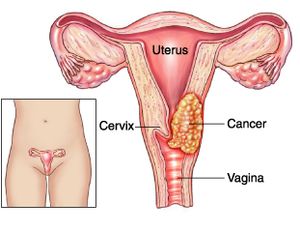
Melanoma develops when the DNA in skin cells is harmed, according to dermatologist Dr. Ahmad Chaudhry of the United Kingdom, who spoke to us.
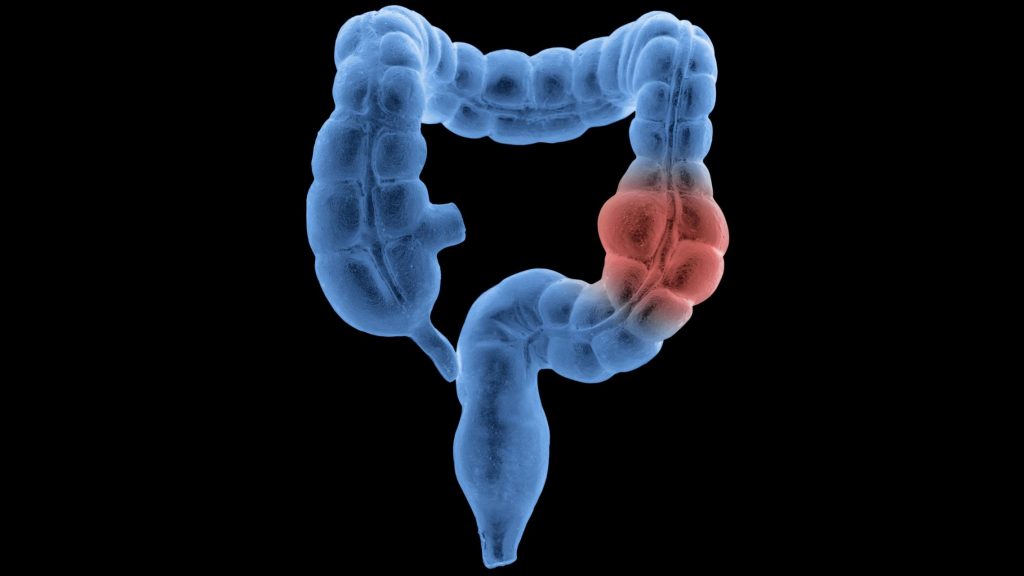
According to Chaudhry, exposure to ultraviolet (UV) light from the sun or tanning booths is frequently to blame for this. “Due to this damage, the melanocytes (cells that produce melanin) proliferate out of control and aggregate into a mass of malignant cells. The development of melanoma in the eyes or internal organs does occur occasionally, but it is less frequent.”
While there are some hereditary risk factors that can potentially play a role, sunshine and tanning beds are linked to skin cancer for a reason.
We were informed by Dr. Sudarsan Kollimuttathuillam, a medical oncologist and haematologist at the City of Hope cancer research organization’s Huntington Beach and Irvine Sand Canyon locations, that 7% to 15% of people with melanoma also have a family member who has the condition.
According to him, having characteristics like pale skin, freckles, or blonde or red hair raises one’s overall risk of developing skin cancer. Atypical mole syndrome is another genetic disorder that dramatically raises the lifetime risk of melanoma and is characterized by a high number of moles with odd forms or color.
Risk can be reduced, but genetics cannot be changed. Doctors advise limiting exposure to the sun during peak hours, staying away from tanning beds in general, and wearing sun protection when outdoors to reduce your risk of acquiring skin cancer.
In the words of Kollimuttathuillam, “regular skin examinations by both you and a dermatologist will help detect melanoma at an early stage, when it is more treatable.”
Experiencing melanoma
One of the most prevalent types of cancer are skin malignancies like melanoma.
More than 97,000 Americans are expected to receive melanoma diagnoses in the US in 2023, according to the American Cancer Society.
As previously mentioned, melanoma can be detected early by a number of telling indications, including genetics and moles. The following procedure usually entails removing and then examining the mole if a doctor suspects it may be malignant. Melanoma presence or absence can be assessed by a range of tests.
It’s crucial to get an early diagnosis of melanoma because it spreads quickly.
According to Kollimuttathuillam, melanoma is the type of skin cancer that is most likely to spread to distant organs or bones. Because of this, imaging technologies may be utilized to spot cancer cells that have done so.
After receiving a melanoma diagnosis, a patient has a variety of treatment choices at their disposal, including radiation therapy, surgery, and immunotherapy.
In the earliest stages of melanoma, patients typically do not require imaging tests because, as Kollimuttathuillam noted, “we know that the best way to stop cancer is to prevent it.” “I cannot emphasize enough how crucial it is for patients to be advocates for their skin health to avoid advanced stages of this disease,” the doctor said.
Types of Immunotherapy
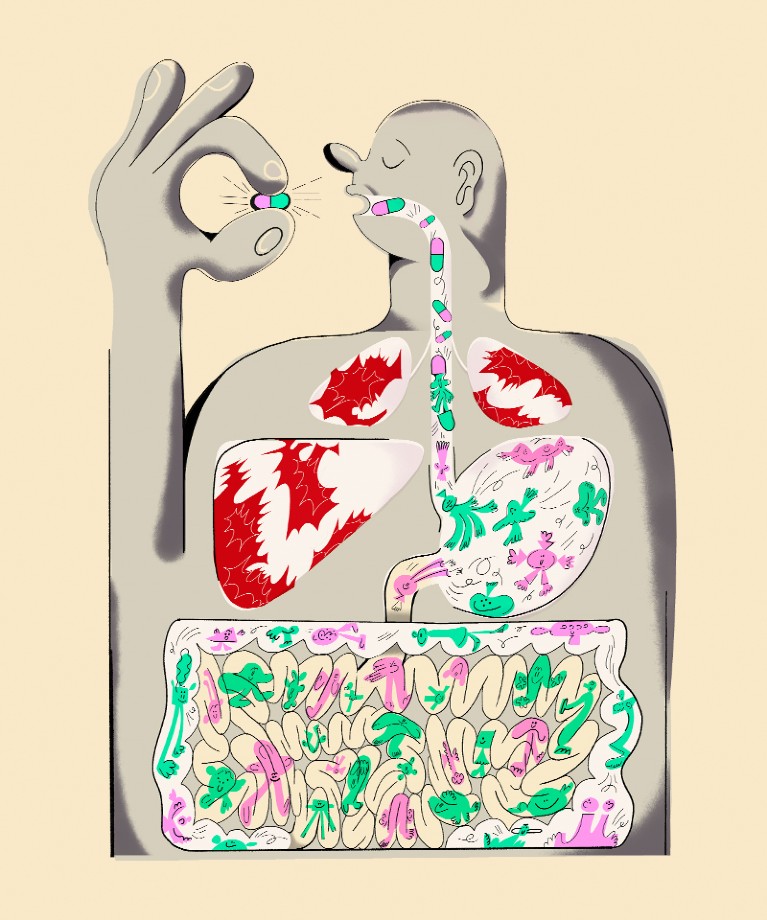
Medication is used in immunotherapy to boost your immune system. This might aid in its attack on cancer cells.
Severe melanoma is treated with a variety of immunotherapies, including:
Checkpoint blockers. The PD-1 blockers nivolumab (Opdivo) and pembrolizumab (Keytruda) as well as the CTL4-blocker ipilimumab (Yervoy) are among these drugs. These medications could aid T cells in your immune system in identifying and eliminating melanoma cancer cells.
Oncolytic virus therapy. In this procedure, melanoma tumors are injected with talimogene laherparepvec (T-VEC, Imylgic), a modified virus. In addition to killing cancer cells, this virus may also cause your immune system to fight cancer cells.
Cytokine therapy. Immune cells can interact with one another with the aid of a class of proteins called cytokines. Interleukin-2 (aldesleukin, proleukin) therapy may enhance your immune system’s defense against cancer.
Your doctor may recommend a single immunotherapy treatment or a cocktail of immunotherapy medications. They might prescribe Yervoy and Opdivo combined, for instance.
Individuals with stage 4 melanoma now have better survival rates thanks to immunotherapy. However, there is a chance that this treatment will have negative side effects.
Contact your doctor straight away if you suspect any potential side effects.
REFERENCES:
- https://www.medicalnewstoday.com/articles/melanoma-targeting-protein-may-boost-skin-cancer-immunotherapy
- https://www.news-medical.net/news/20230705/New-protein-found-to-help-melanoma-evade-the-immune-system.aspx
- https://www.cancer.org/cancer/types/melanoma-skin-cancer/treating/immunotherapy.html
- https://www.healthline.com/health/skin-cancer/treatment-options-stage-4-melanoma
For Skin cancer medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=10