Best ways to treat and relieve your tired eyes.
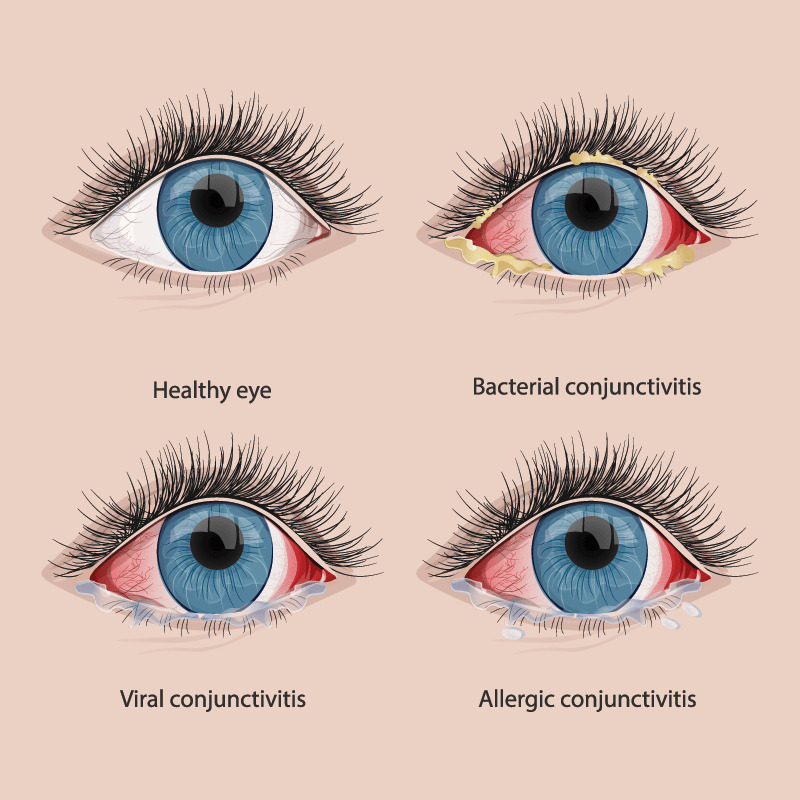
Eyes that are tired may appear bloodshot, bloated, or puffy. What causes eye fatigue? A multitude of factors, such as allergies, lack of sleep, nutrition, and digital eye strain, can make your eyes look and feel tired.

Making adjustments to your daily routine or environment is the typical course of treatment for eyestrain. Some individuals might require care for an underlying eye issue.
For some people, wearing glasses that are prescribed for specific activities, such as for computer use or for reading, helps reduce eyestrain. Your eye specialist may suggest that you take regular eye breaks to help your eyes focus at different distances.
Get a few of your tea bags.
Black or green tea’s caffeine may help with dark circles by constricting blood vessels and lowering blue colouring. Moreover, these caffeinated teas can eliminate bloating by pulling out fluid.
But use rooibos (red tea) or chamomile if you want a more calming effect for itchy skin.
Instructions:
- For two to four minutes, steep two tea bags in a mug of hot water.
- After removing the tea bags, squeeze any remaining water out of them.
- The tea bags can be chilled for ten minutes in the refrigerator or allowed to slowly cool at room temperature.
- Spend 15 minutes with the bags resting over your closed eyes.
- Never leave them on for more than 30 minutes at once.
Reach into the coffee maker
While a caffeine fix for the skin might also assist reduce blotchiness or puffiness, your cold brew might provide you a refreshing jolt. With an ice cube tray, start by freezing some freshly made coffee. When the coffee ice is ready, rub one ice cube for a few seconds:
- beneath your eyes
- between your brows
- across your nose’s bridge.
- from your eye’s outer corners to your temples
Try the 100% Pure Coffee Bean Caffeine Eye Cream as well. Reviewers give this product 4.5 stars and claim it can help alleviate crow’s feet and keep eyes hydrated.
Get a cucumber from your crisper.
Vitamin C and folic acid, which are both abundant in cucumbers, aid to promote cell growth and protect against environmental damage. The final outcome? Reduced puffiness, inflammation, and discolouration under your eyes.
Instructions:
- Cut a cucumber into two half-inch-thick slices.
- For about 15 minutes, place the slices over your closed eyes.
- Instead, try using cold spoons. They can aid in blood vessel constriction and lessen dark circles beneath the eyes.
Try the Yes to Cucumbers Soothing Eye Gel as well. Reviewers indicate that while this gel may be too harsh for people with sensitive skin, it nevertheless performs better than more expensive creams.
Massage your eyes with a tap.
You can improve lymph outflow by gently tapping your brows, cheekbones, and eye sockets with your index and middle fingers in a circle. This might lessen inflammation and even out skin tone.
Instructions:
- Spend at least 30 seconds massaging your eyes while using an eye cream.
- Embrace the pressure, but don’t rub or push too hard.
Think about eye cream
Must you shell out a lot of money for a nice balm? The simplest response is no about dark circles.
However, you might experiment with more reasonably priced moisturising salves that contain tea, coffee, or cucumber extract; some of these treatments may also assist to lessen the visibility of fine lines and wrinkles.
For a boost, apply under-eye patches.
A more recent fad for treating the skin around your eyes is under-eye patches. They are adorable and perfect for Instagram, but many people also find them to be useful. Just be aware that they provide more of a short fix—if you will, a helping hand after a wild night out.
Unsure on how to choose your patch? Use components like retinol and hyaluronic acid that are gentle on the eyes. Check out our list of the top choices to pack your suitcases as well.
Pick up the concealer that corrects colours.
Marcus clarifies that concealers merely assist in hiding dark circles. In other words, they won’t contribute to the reduction of puffiness. She advises combining an eye cream with concealer because of this: Use an eye cream to help with both the symptoms and the cause, and then cover up any remaining darkness with concealer.
On moisturised skin, concealer will go on more smoothly, she says. Hence, using a moisturising eye cream before applying concealer helps prepare the skin.
Concealer by itself can still be effective in an emergency. So, grab a tiny amount of color-correcting concealer the next time an important meeting or function sneaks up on you.
Try:
- if you have a darker skin tone, orange.
- you might have lighter skin, wear pink.
- If your circles often appear overly purple, use yellow.
Why do we get dark circles or puffiness?
Genetics is the biggest explanation for this, especially for those of you who have exhausted all other options.
If you have periorbital hyperpigmentation, often known as dark circles under the eyes or sunken eyes, you may be genetically predisposed to the condition. Similar to hereditary face features, you can also have permanent under-eye pouches.
Here’s why certain qualities are highlighted.
Eyes under bags
When the tissue there fills with water, the lower lids and bags become puffy. An increase in fluid retention in that region can be brought on by the fatty tissue retained within the socket and upper lid thinning out with age.
While looking in the mirror first thing in the morning, puffiness is frequently the most noticeable. That’s because during sleep, fluid has an opportunity to collect. Once you’ve been vertical for a while, bags usually start to disappear.
Shady circles
Despite the fact that there are numerous causes for dark circles, those around the eyes often have a somewhat darker complexion simply because the area’s thinner skin is stretched over a collection of purple blood vessels and muscle.
Prevent tired eyes
Extend your time in bed
Cut your late-night Netflix session short, or try to get as much rest as you can. Prop your head up a little bit while you sleep if you continue to experience morning eye puffiness or blue colouring.
Marcus notes that sleeping with your head slightly elevated can aid in avoiding fluid buildup in the periorbital region. Before going to bed, take off any makeup to prevent smearing it in your eyes and aggravating the skin around them.
Apply a cool towel.
To help with the “I just woke up” look, Marcus advises placing a cool washcloth over your eyes. She claims that this reduces puffiness and skin discolouration by generating vasoconstriction (constriction of blood vessels).
Also, it can have a calming impact all around, and you won’t need to search your refrigerator for fresh cucumbers.
Do some eye exercises.
Marcus claims that eye strain can make eyes fatigued by reducing the flow of naturally lubricating tears and causing dry eyes.
“Taking regular breaks from screen time and completing eye exercises may help minimise eye strain and, as a result, help eyes function normally by releasing lubricating tears, lowering dryness, redness, and bloodshot eyes,” she explains.
Exercise for the eyes can be rather easy. In instance, one exercise merely requires you to change your focus while sitting. Here, pick up a handful of these basic techniques. Moreover, face yoga (yes, it exists) can help lessen eye strain.
Adapt the lighting and gadget displays.
According to Marcus, taking breaks from screen time to prevent eye strain can also be beneficial.
Keeping your phone or tablet in night mode reduces exposure to blue light, which can enhance the quality of your sleep, the expert continues.
Put on your blue light spectacles.
Blue light glasses may reduce the strain if night mode isn’t effective in preventing your tablet or device from gleaming brightly like a diamond.
Breaks from the screen
According to Marcus, prolonged screen usage might strain the eyes. This occurs in part as a result of the blood vessels around your eyes enlarging, which can cause dark circles, as you would have imagined.
Let your eyes to take little breaks for a much-needed vacation:
- Give the 20/20/20 rule a try. Every 20 minutes, look away from your screen. Focus for 20 seconds on a distant object that is at least 20 feet away.
- Move and stand up. Spend at least five minutes standing up, stretching, and moving about after each hour of screen usage.
REFERENCES:
- https://www.healthline.com/health/beauty-skin-care/make-eyes-look-more-awake
- https://www.webmd.com/eye-health/ss/slideshow-relieve-tired-eyes
- https://www.mayoclinic.org/diseases-conditions/eyestrain/diagnosis-treatment/drc-20372403
- https://www.healthshots.com/preventive-care/self-care/eye-fatigue-how-to-prevent-relieve-tired-eyes/
- https://www.allaboutvision.com/conditions/ways-relieve-tired-eyes/
For more details, kindly visit below.