Women with depression face higher cardiovascular disease risk than men
According to experts, inflammation and hormones in the body are two things that can lead to the development of cardiovascular disease. They claim that when it comes to screening for depression, medical professionals should do a better job of looking at both men and women. After receiving a diagnosis of depression, women are much more likely than men to develop cardiovascular disease.
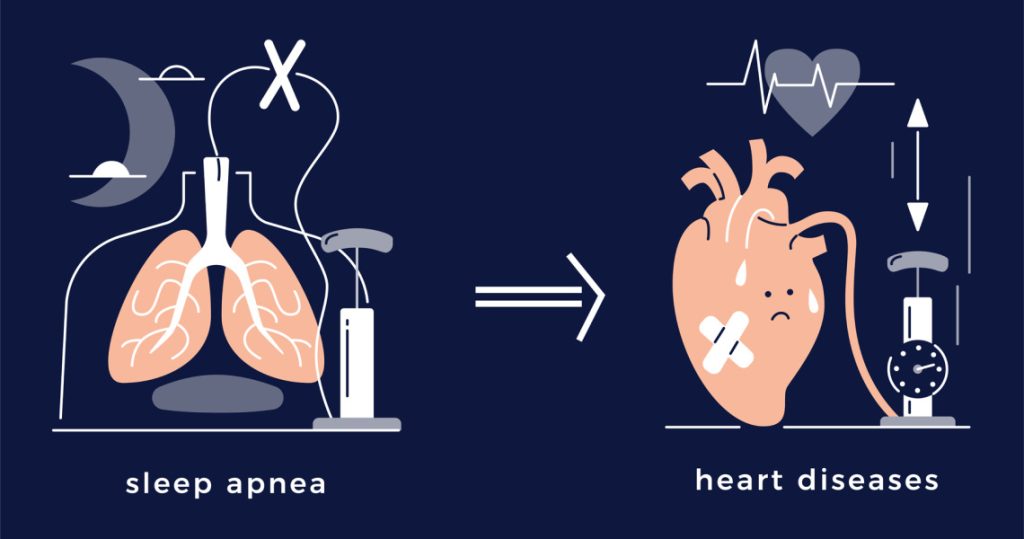
Heart attacks, strokes, heart failures, and atrial fibrillation are all considered forms of cardiovascular disease, or CVD. Women in the United States are twice as likely as men to experience depression, and over 60 million women are thought to have heart disease. According to a recent study, cardiologists might want to devote more time to screening patients for depression. Improved comprehension will enable medical professionals to provide depression treatment that is optimal for men and women, improving the outcomes of CVD for these populations.
Between 2005 and 2022, the study monitored and examined medical claims, examining the rates of depression and eventual diagnosis of cardiovascular disease in over 4 million patients. Men made up slightly more of the study’s participants than women. The mean age was forty-four. Before being diagnosed with CVD, the participant had to receive a clinical diagnosis to be eligible for a depression status in the analysis. Body mass index, blood pressure, fasting cholesterol, and blood glucose levels were among the patient health data. Cardiovascular events included atrial fibrillation, heart failure, angina pectoris, and myocardial infarction, or heart attack. Multiple hazard ratios, which simply show a person’s risk of something occurring in men versus women, were calculated by researchers using data.
According to the data, the risk ratio for a diagnosis of depression to result in cardiovascular disease was 1 point 64 for women and 1 point 39 for men. Women were more likely than men to experience depression that directly resulted in heart attacks, chest pain, strokes, heart failure, and other incidents. Researchers acknowledged that there were several obvious limitations to the study. One of the challenges they faced was the inability to obtain precise information regarding the depression symptoms of the participants or the possible impact of COVID-19. Furthermore, because the study was observational in nature, it was unable to prove a link between depression and CVD.
Although heart attacks are more commonly associated with men than women in society and the media, both sexes are equally at risk. For women, however, the odds of surviving a heart attack and receiving treatment are not as good. While she wasn’t involved in the study, Dr. Evelina Grayver, a cardiologist and the director of Women’s Heart Health at Central Region Northwell Health, expressed her happiness that research is finally being done on the topic and pointed out several important points. According to Grayver, Medical News Today, the leading cause of death for women is cardiovascular disease. More women die from it than from lung, breast, and colon cancer combined.
However, because women do not usually exhibit the symptoms of a heart attack, a great deal of them choose to ignore their symptoms. According to Grayver, women are more likely to experience exhaustion, tightness in the chest, and discomfort in the abdomen rather than pain in the left arm or the feeling of an elephant resting on their chest. Women are 20 percent more likely than men to pass away during the first five years following a severe heart attack, according to previous research from the American Heart Association. It also mentions that women were less likely to have a cardiologist visit them in the hospital and to be prescribed drugs like beta blockers and cholesterol lowers.
Compared to men, women are diagnosed with depression twice as frequently. Why is the key question? According to the new study’s researchers, women might have more severe and enduring symptoms. This heightened intensity may have an additional impact on lifestyle choices that raise an individual’s risk of having a heart attack. Women also experience more particular health difficulties during menopause and pregnancy. Hormonal fluctuations have the potential to exacerbate mental health conditions like anxiety, depression, and overall stress. The metabolic syndrome, which includes traditional CVD risk factors like high blood pressure, diabetes, and obesity, is also substantially more common in women.
REFERENCES:
Medications that have been suggested by doctors worldwide are available here
https://mygenericpharmacy.com/index.php?therapy=11