Crohn’s disease: Top bad thing to your digestive system.
Inflammatory bowel illness includes Crohn’s disease (IBD). It results in the tissues in your digestive tract swelling (inflammation), which can cause abdominal pain, severe diarrhoea, exhaustion, weight loss, and malnutrition.
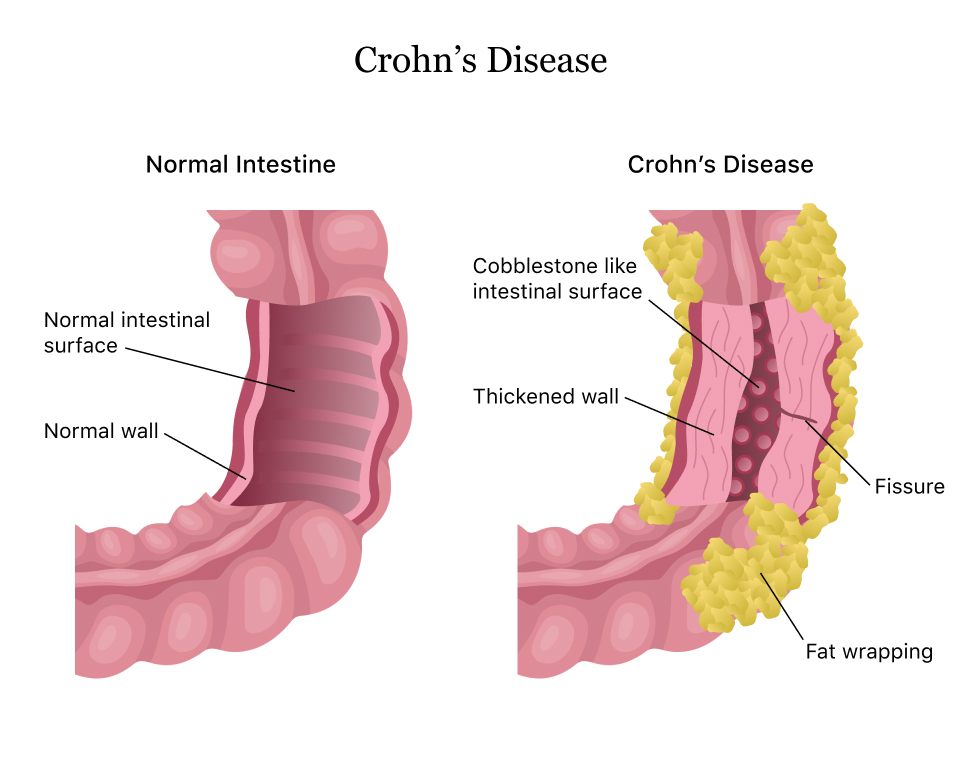
People with Crohn’s disease may experience inflammation in many parts of their gastrointestinal tract, most frequently the small intestine. This inflammation frequently penetrates the innermost layers of the bowel. The symptoms of Crohn’s disease can occasionally be life-threatening and can be both unpleasant and incapacitating.
Although there is no proven treatment for Crohn’s disease, medicines can significantly lessen its signs and symptoms and even result in long-term remission and inflammatory healing. With medication, many Crohn’s disease sufferers can lead productive lives.
Types of Crohn’s disease
Different parts of the digestive system may be impacted by Crohn’s disease. The following list includes many forms of Crohn’s disease:
- Ileocolitis: Inflammation affects the small intestine and a portion of the colon’s big intestine. Crohn’s disease most frequently manifests as ileocolitis.
- Ileitis: The small intestine swells and becomes inflamed (ileum).
Gastroduodenal: The stomach and the top of the small intestine are both affected by inflammation and irritation (the duodenum). - Jejunoileitis: Patchy inflammation appears in the top portion of the small intestine (called the jejunum).
Who might get Crohn’s disease?
The cause of Crohn’s disease is unknown. Your likelihood of getting the illness may be impacted by a number of variables, including:
- Autoimmune disease: Your immune system may attack healthy cells as a result of digestive tract bacteria.
- Genes: Inflammatory bowel disease(IBD) is a genetic condition that frequently runs in families. You may be more likely to get Crohn’s disease if one of your parents, siblings, or other family members does. People who have a number of certain gene mutations (changes) may be predisposed to Crohn’s disease.
- Smoking: Smoking cigarettes could more than double your risk of developing Crohn’s disease.
These kinds of infections can become worse due to immune system issues caused by Crohn’s disease and associated therapies.
Yeast infections, which can harm the lungs and the digestive system, are frequent in people with Crohn’s disease. To avoid further difficulties, it’s crucial that these infections are correctly recognised and treated with antifungal drugs.
Crohn’s symptoms
Crohn’s disease signs and symptoms frequently appear gradually. Over time, some symptoms could possibly deteriorate more. Although it’s possible, it’s uncommon for symptoms to appear out of the blue. The following are some of the first signs of Crohn’s disease:
- diarrhoea
- stomach pains
- stool with blood
- fever
- fatigue
- reduced appetite
- slim down
- after having a bowel movement, you still feel like your bowels aren’t empty.
- feeling the desire to go to the bathroom a lot
These symptoms can occasionally be confused with those of a different illness, such as food poisoning, an upset stomach, or an allergy. If any of these symptoms continue, you ought to visit your physician.
As the illness worsens, the symptoms could get worse. More problematic signs could be:
- a discomfort and drainage-causing perianal fistula close to your anus
- Anywhere from the mouth to the anus, ulcers may develop
- swelling of the skin and joints
- breathing difficulties or a reduced capacity for exercise as a result of anaemia
Early identification and detection can help you prevent serious problems and start treatment sooner.
Outlook
More efficient therapies and perhaps even a cure for Crohn’s disease are still being sought for by researchers. However, symptoms can be well controlled, and remission is conceivable.
Your doctor can help you locate the proper prescription drugs, complementary therapies, and lifestyle changes that can be beneficial.
Consult your doctor if you experience gastrointestinal symptoms to identify the source and any relevant treatments.
REFERENCES:
- https://www.mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304
- https://my.clevelandclinic.org/health/diseases/9357-crohns-disease
- https://medlineplus.gov/crohnsdisease.html
- https://www.healthline.com/health/crohns-disease
- https://www.medicalnewstoday.com/articles/151620
For more details, kindly visit below.