Quick survey on Paralysis and its different types.
What is Paralysis?
Loss of muscle function in the body is referred to as paralysis. Sometimes paralysis is transitory, and occasionally it is permanent. While paralysis can affect any portion of the body, the majority of cases are seen in the limbs. Paralysis, both partial and total, can happen at any time. There is no immediate pain experienced by a patient who is paralysed.
The treatment plan is designed to either cure or treat the condition, depending on the nature of the underlying cause, in order to prevent the patient’s everyday lifestyle from being significantly impacted.
The most frequent underlying cause of partial or total paralysis in a patient is a stroke. Incomplete paralysis means the patient has no control over the afflicted muscle tissue while partial paralysis means the patient still has some control over the affected muscle.
Types and causes of Paralysis
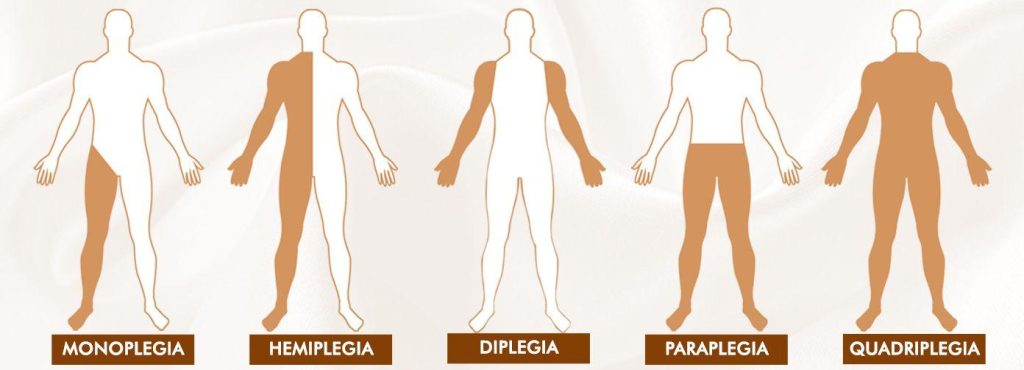
The paralysis types that are best known to the public are:
- Monoplegia
- Hemiplegia
- Paraplegia
- Quadriplegia
- lock-in Syndrome
Monoplegia:
Monoplegia is a form of paralysis in which a person is unable to control one limb. The paralysis frequently affects just one arm, or occasionally only particular arm muscles. A common side effect of cerebral palsy is monoplegia. The brain’s capacity to control some body muscles is lost in cerebral palsy. The majority of cerebral palsy patients are young children and teenagers.
Since the patient can still do his everyday activities with only one limb paralysed, monoplegia is regarded as a positive indicator in the prognosis of this illness.
Hemiplegia:
Hemiplegia is a form of paralysis in which one side of the body loses control. This usually only has an impact on one arm or limb, though it might occasionally also have an impact on the torso. Hemiparesis is a condition in which a person’s functional use of their limbs is greatly diminished in terms of strength and endurance, but they retain some degree of functional use. In a few situations, hemiparesis progresses to hemiplegia.
When the corpus callosum between the left and right sides of the brain is damaged, hemiplegia can result. It can also result from spinal cord injury. A stroke, which impairs one side of the brain’s functionality, can also result in hemiplegia.
Left and right hemiplegia are additional divisions of hemiplegia. The diagnosis of right or left hemiplegia depends on where the injury is located.
Paraplegia:
In the case of paraplegia, the patient is unable to control their muscles below the waist. Each person experiences paraplegia differently. The fundamental cause of paraplegia typically arises in the brain or spinal cord, and people who experience it have completely normal legs. Sometimes a lower torso limb only has partial paraplegia, while other times it occurs completely. Regular physical therapy and medication are frequently responsible for partial paraplegia.
Paraplegia frequently results from a patient suffering from a brain, spinal cord, or both types of injuries. The impulses that the brain sends to the lower body are not returned to the brain through the spinal cord in paraplegic patients. Patients who suffer from this absence of brain communication not only lose their ability to move, but also their ability to feel.
A patient with partial or incomplete paraplegia may still be able to use one leg, whereas a patient with complete paraplegia loses sensation and use of both legs.
Quadriplegia
All four limbs of the body are paralysed in a quadriplegia. In this scenario, the patient’s hands and legs become impaled as a result of the brain’s signals to the areas below the neck not being returned. Sending and receiving signals from the brain is the responsibility of the spinal cord. This stops working in quadriplegia, resulting in the condition.
Quadriplegia may begin as a result of spinal cord or brain injuries. The likelihood of recovery from this condition increases as the wounds to the afflicted area heal or as the brain inflammation subsides. It is impossible to provide an accurate forecast, though.
In addition to exhaustion, sudden spasms, lack of sensation below the neck, trouble passing urine from the body, respiratory distress, bedsores, and depression, patients with quadriplegia also experience fatigue.
Locked-in Syndrome:
In a condition known as “Locked-in Syndrome,” the patient is unable to control any area of their body with their under-eye muscles. Locked-in syndrome is primarily a consequence of a serious brain damage, a stroke, or brain cancer. A person suffering from locked-in syndrome won’t be able to move any of his body’s limbs or his lips, jaw, or up and down or side to side movements in the neck. However, those who experience locked-in syndrome are still able to blink and move their eyes up and down.
Doctors rely on the moment of the eyes to make a precise diagnosis because locked-in syndrome frequently mimics the symptoms of a coma.
To ensure that the patient gets all the nutrients needed, adequate nutrition is essential. However, the patient must be fed through a stomach tube, which must either be inserted directly into the stomach through an incision made in the small intestines or through the nose.
Patients who spend a lot of time in bed can develop pressure sores, blood clots, damaged muscles, and damaged nerves. By moving the patient, rubbing the muscles, rotating the joints along their axes, and using physiotherapy, care should be given to prevent pressure sores.
Complications of paralysis
Other physiological processes including respiration and heart rate might be impacted by paralysis. Other body systems in the affected area may also be affected by the illness. Depending on the kind of paralysis you have, you could be vulnerable to:
- breathing issues, coughing, and pneumonia risk.
- Deep vein thrombosis (DVT) and clots in the blood.
- issues with speech or swallowing (dysphagia).
- both anxiety and depression.
- Sexual difficulties and erectile dysfunction.
- Excessively high blood pressure (autonomic dysreflexia) or low blood pressure (orthostatic hypotension) and heart problems.
- bowel incontinence and urinary incontinence.
- Sepsis and pressure wounds (bedsores).
How is paralysis diagnosed?
Paralysis is frequently simple to diagnose, particularly when your lack of muscle function is visible. Your doctor may employ X-rays, CT scans, MRI scans, or other imaging techniques to examine inside body parts where paralysis is more challenging to detect.
If you suffer a spinal cord injury, your doctor might perform a myelogram to determine how you are doing. In this surgery, a particular dye will be injected into the spinal cord’s nerves. This will make it easier for them to see your nerves on X-rays. In addition, they might conduct an electromyography. They will utilise sensors to assess the electrical activity of your muscles during this operation.
How is paralysis treated?
The underlying cause of the paralysis as well as the symptoms present will determine a therapy strategy. For illustration, a physician would advise:
- operation or potential amputation
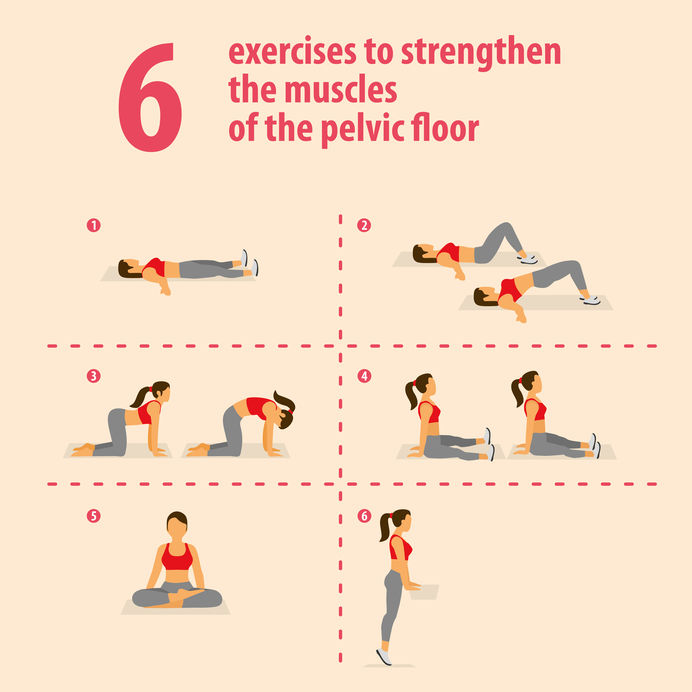
- physical exercise
- Workplace therapy
- wheelchairs, braces, portable scooters, and other mobility aids
- If you have spastic paralysis, you may take drugs like Botox or muscle relaxants.
Paralysis is frequently incurable. However, a medical team might suggest a range of medications, equipment, and tactics to assist manage symptoms.
REFERENCES:
- https://www.healthline.com/health/paralysis
- https://www.medicalnewstoday.com/articles/paralysis
- https://my.clevelandclinic.org/health/diseases/15345-paralysis
- https://www.narayanahealth.org/paralysis
For more details, kindly visit below.