Is BMI not accurate to predict obesity in many people?
Body mass index (BMI) is a common metric used in healthcare facilities to determine patient health.
It has been frequently criticized for its simplicity of what being healthy actually entails while being used for decades as the standard measurement for health based on body size.
In fact, many people argue that BMI should not be utilized in medical or fitness settings since it is antiquated and inaccurate.
What is BMI?
“BMI” is an acronym for “body mass index.” A Belgian mathematician by the name of Lambert Adolphe Jacques Quetelet created the BMI in 1832.
He created the BMI scale to help governments allocate health and financial resources by swiftly estimating the level of overweight and obesity in a specific community.
Interestingly, Quetelet claimed that BMI was better at capturing the general health of a group than using it to investigate a single individual. Even so, it’s frequently used to gauge people’s health.
The BMI scale is based on a mathematical formula that compares a person’s height in meters squared to their weight in kilograms to determine whether they are a “healthy” weight:
Height (m2) / weight (kg) equals BMI.
Alternately, you can determine BMI by multiplying 703 by the product of your weight in pounds and your height in square inches:
Weight (lbs) x Height (in2) x 703 equals BMI.
A BMI calculator online, like the one offered by the National Institutes of Health, is another option. If you fall within the “normal” weight range, your BMI is calculated and then compared to the BMI scale.
If you don’t fit the definition of “normal” weight, a healthcare practitioner might recommend health and lifestyle adjustments to you.
To more accurately reflect the size and stature of their inhabitants, some nations have adopted the BMI scale. For instance, Asian men and women have been found to have a higher risk of heart disease than non-Asians at lower BMIs.
Even though this can give a healthcare practitioner a quick overview of a person’s health based on weight, it ignores other aspects of a person’s health, including age, sex, race, genetics, fat mass, muscle mass, and bone density.
Is it a reliable sign of health?
The majority of research demonstrates that a person’s risk of chronic disease and early mortality does increase with a BMI lower than 18.5 (“underweight”) or 30.0 or above (“obese”), despite concerns that BMI doesn’t precisely indicate if they are in good health.
A 2017 retrospective research of 103,218 fatalities, for instance, discovered that those with a BMI of 30.0 or higher (referred to as “obese”) had a 1.5–2.7-fold higher chance of dying following a 30-year follow-up.
Another study with 16,868 persons found that those with an “obese” BMI had a 20% higher chance of dying from any cause and heart disease than those with a “normal” BMI.
Additionally, the researchers discovered that people with “underweight” BMIs and “severely obese” or “extremely obese” BMIs died on average 6.7 years and 3.7 years earlier than people with “normal” BMIs.
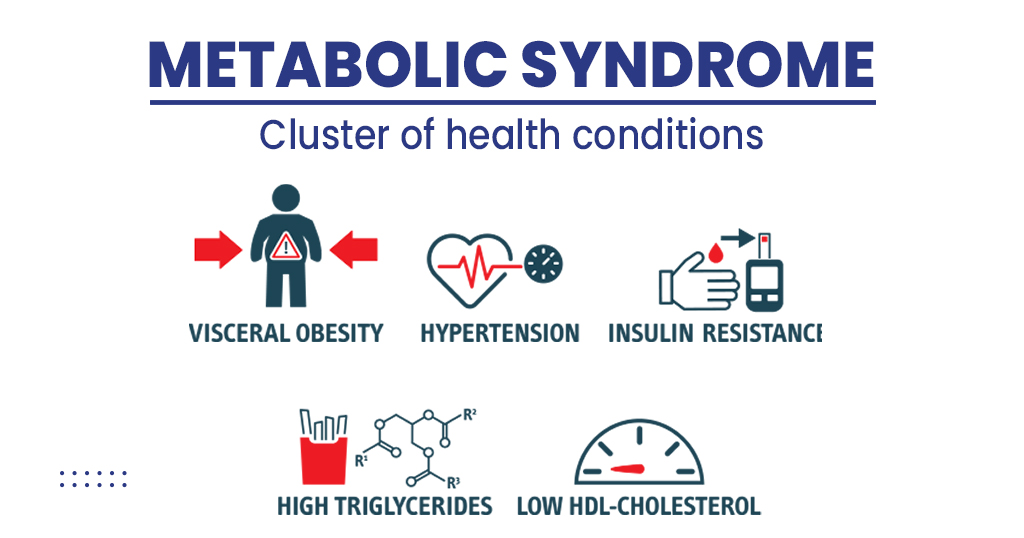
According to other research, a BMI over 30.0 considerably raises the chance of developing chronic conditions such as type 2 diabetes, heart disease, breathing problems, renal illness, non-alcoholic fatty liver disease, and mobility problems.
A person’s risk of developing metabolic syndrome, heart disease, and type 2 diabetes has also been shown to drop by 5–10% with a BMI reduction.
Many health practitioners can use BMI as a broad indicator of a person’s risk because the majority of studies indicate that obese persons have an elevated chance of developing chronic diseases. But it shouldn’t be the only diagnostic instrument employed.
The BMI as a measure of obesity
The National Health and Nutrition Examination Survey (NHANES), which was conducted from 2011 to 2018, had data on 9,784 participants with an average age of 39.
BMI and body fat % were determined using dual-energy x-ray absorptiometry (DEXA) in the data. BMIs were divided into categories according to ethnicity.
In the end, 36% of individuals were obese, defined as having a BMI of 30 or more. However, 74% of participants were rated as obese based on their body fat percentage.
When body fat % was taken into account, many persons with BMIs between 18.5 and 24.9, which are considered healthy weights, were labelled as obese, including:
- 27% of Black non-Hispanics
- 44% of white non-Hispanics
- 49 percent of Hispanics
- In Asia, 49%
The finding that non-Hispanic Black people with overweight had 58% lower risk of obesity than non-Hispanic White people struck me as particularly fascinating. Dr. Erkeda de Rouen, a board-certified specialist in family, diversity, and lifestyle medicine who was not involved in the study, said that this might be caused by the regular genetic weight distribution.
A person’s mental health and complex sociological issues like money, access to affordable and nutritious food, food skills and knowledge, and housing conditions are all ignored when a person’s health is solely determined by their BMI.
Drawbacks of BMI
There are many problems with the use of BMI, despite data linking low (below 18.5) and high (30 or above) BMI with elevated health risks.
Disregards other potential health factors
Without taking into account a person’s age, sex, genetics, lifestyle, medical history, or other considerations, BMI just provides a “yes” or “no” answer as to whether they are of “normal” weight.
Relying just on BMI could lead to an overestimation or underestimation of a person’s genuine state of health by excluding other crucial health indicators including cholesterol, blood sugar, heart rate, blood pressure, and inflammation levels.
In addition, BMI employs the same formula for both sexes even though men and women have different body compositions, with males having more muscle mass and less fat mass than women.
Additionally, a person’s body fat mass naturally rises and their muscle mass naturally reduces as they age. Numerous studies have demonstrated that an older adult’s BMI of 23.0-29.9 can be protective against disease and early death.
The premise that all weight is equal
Muscle is denser and takes up less space even though 1 pound or kilogram of muscle weighs the same as 1 pound or kilogram of fat. As a result, someone who is extremely slim but has a lot of muscle may weigh more than average.
For instance, a person with a BMI of 29.5 who weighs 200 pounds (97 kilograms) and is 5 feet 9 inches (175 cm) tall is considered to be “overweight.”
The appearance of two people who are the same height and weight might vary greatly. One can be a bodybuilder with a lot of muscle, whilst the other might have more fat.
If BMI is the only factor taken into account, it is quite easy to mistakenly label someone as “overweight” or “obese” despite their low-fat mass. Therefore, in addition to a person’s weight, it’s necessary to take their bone, muscle, and fat mass into account.
Overlooks the distribution of fat
Even while a higher BMI is associated with worse health outcomes, the distribution of body fat may be more important.
People with a gynoid or pear-shaped body type, also known as those who have fat accumulated in their hips, buttocks, and thighs, are less likely to develop chronic disease than people with an android or apple-shaped body type.
For instance, researchers discovered that those with an apple-shaped fat distribution had a substantially higher risk of all-cause mortality than those with a pear-shaped distribution in a study of 72 studies that included data from more than 2.5 million people.
The authors really emphasized that BMI does not take into account where fat is stored in the body, which might cause a person to be incorrectly classified as being sick or at risk for disease.
Possible weight bias
The medical professional is expected to apply their best judgment, which means that they will take the BMI result and treat each patient as an individual.
However, some medical practitioners simply utilize BMI to assess a patient’s health before making recommendations, which can result in weight prejudice and subpar medical care.
Higher BMI patients more frequently claim that their doctors only address their BMI during appointments for unrelated issues. Serious medical conditions frequently go undiagnosed or are misdiagnosed as weight-related disorders.
In reality, research has shown that those with higher BMIs are less likely to get frequent health checks because of anxiety about being assessed, mistrust of the medical staff, or a bad experience in the past. This can result in delayed diagnoses, care, and treatment.
It might not apply to all populations
Even though BMI is widely used among all adults, it could not adequately reflect the health of some racial and cultural groups.
For instance, multiple studies have demonstrated that, compared to white individuals, people of Asian descent have a higher risk of chronic disease at lower BMI cut-off points.
In truth, the Asian-Pacific BMI recommendations, which offer different BMI cut-off points, were created by the World Health Organisation.
Numerous research has demonstrated that these alternate cut-off points are more effective at identifying Asian populations’ health risks. However, further research is required to compare these cut-off points with Asian Americans who are multigenerational.
Additionally, despite having higher muscle mass and lower fat mass, Black persons may be mistakenly labeled as overweight. This may imply that Black women, in particular, have a greater BMI cutoff criterion for chronic illness risk than those of other races.
Indeed, a 2011 study indicated that Black women were deemed metabolically healthy at cut-off points 3.0 kg/m2 higher than non-Black individuals, which further calls into doubt the applicability of BMI to all racial and ethnic groups.
Last but not least, depending solely on BMI disregards the cultural significance of body size to various communities. Higher fat mass is regarded as desirable and healthier in some cultures. Healthcare practitioners should take into account what each person’s definition of “health” is.
The conclusion
Body mass index (BMI) is a highly debatable health assessment technique used to determine a person’s risk for poor health and body fat.
According to most studies, as BMI rises above the “normal” level, there is an increased risk of developing a chronic illness. Additionally, a low BMI (below 18.5) has been associated with negative health effects.
However, BMI does not take into account other factors that may affect health, including age, sex, fat mass, muscle mass, race, genetics, and medical history. Furthermore, it has been demonstrated that using it as the only predictor of health increases weight bias and health disparities.
BMI is a good place to start, but it shouldn’t be the primary indicator of your health.
REFERENCES:
- https://www.medicalnewstoday.com/articles/bmi-not-accurate-in-predicting-obesity-in-majority-of-people-study-finds
- https://www.healthline.com/nutrition/is-bmi-accurate
- https://www.health.com/high-bmi-metabolic-health-7370003
For Obesity medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=20