Melanoma: Black man at 26% higher risk to die.
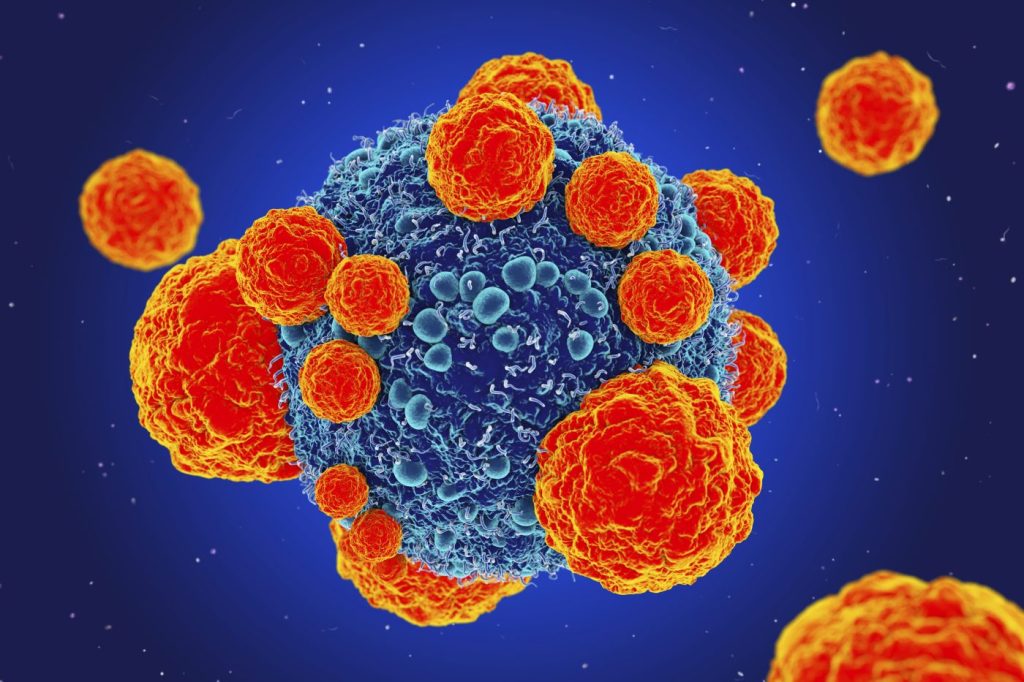
Significant melanoma discrepancies between racial and ethnic groupings have been discovered by researchers.
Using the National Cancer Database, researchers discovered that Black males had the lowest survival rates for melanoma diagnoses and a 26% higher mortality risk than white men.

Put on sun-protective clothing, use sunscreen, and examine your skin once a month to protect yourself from melanoma.
While there are many studies on both male and female melanoma instances, there is little information on how race affects this skin disease, particularly in men.
A group of experts looked over the National Cancer Database to find out more. They looked at male non-Hispanic white, non-Hispanic black, non-Hispanic Asian, non-Hispanic American Indian/Alaska Native instances of primary cutaneous invasive melanoma.
Their data showed melanoma incidence differences between racial and ethnic groupings.
The trunk was the most typical site for melanoma in both white people and American Indian/Alaskan Native people. Men of color Black, Asian, and Hispanic had their lower extremities found to have melanoma, though.
The majority of stage 3 or stage 4 melanomas (48.6%) were seen in Black people. White guys (75.1%) and Black males (51.7%) had the highest 5-year overall melanoma survival rates.
According to research, black people with melanoma had a 26% higher mortality rate than white people with the same diagnosis.
Dr. Bianka Bubic, study author and a dermatology research fellow at The Ohio State University Wexner Medical Centre, said, “We hope that this study lays the foundation for future research to explore the reasons for why there are different presentations and survival among men of diverse racial groups in melanoma.”
Survival rates for melanoma vary by race
Researchers are currently looking into why Black people have a higher chance of developing severe melanoma. Pigmented lesions that may have variations in size, form, symmetry, or pattern can be early indicators of melanoma.
A board-certified dermatologist at Psoriasis Telehealth in Palo Alto, California, Dr. Faranak Kamangar, told that early detection of skin abnormalities in the Black community may be more challenging, thus postponing diagnosis.
She pointed out that the results emphasise the value of early cancer screening in many racial and ethnic groups.
Dr. Kamanger pointed out that socioeconomic issues such a lack of cheap insurance and medical treatment may disproportionately affect the severity of melanoma in Black communities, which could result in a diagnosis at a late stage.
“The main tendency, that Black men are diagnosed with melanoma at later stages, making it less likely to be treated and probably leading to greater rates of morbidity and mortality for this population, has been known to us for some time. The research also confirms previously reported findings that Black men are more likely to develop acral lentiginous melanoma, a subtype of melanoma that is typically detected at a later stage and may occur in difficult-to-examine body regions. Bob Marley is a well-known illustration. He unfortunately had a late diagnosis of melanoma and passed away from it,” according to board-certified dermatologist Dr. Faranak Kamangar.
Acral lentiginous melanoma is the most prevalent melanoma subtype in Black people, but it is also more challenging to identify and diagnose early.
Dr. Wael Harb, a haematologist and medical oncologist at MemorialCare Cancer Institute at Orange Coast Medical Centre in Fountain Valley, California, said that acral lentiginous melanoma “typically appears on less noticeable or examined areas like the palms, soles, or under the nails.”
Are there genetic factors that influence melanoma risk?
Racial and ethnic inequalities in melanoma risk may also be influenced by genetics.
According to Dr. Kamanger, “Acral lentiginous melanoma has higher rates in this population due to genetic predispositions and, in general, is diagnosed at a later stage.”
We have now discovered genes that predispose to acral lentiginous melanoma, and this is the key factor contributing to greater risk among some groups. Diagnosis may be delayed if the nails and bottom of the feet are involved. Except for the amelanotic subtype, melanoma is often pigmented and brown in colour, according to Dr. Kamanger.
Dr. Harb emphasised that acral lentiginous melanoma frequently manifests in locations that are not as exposed to the sun. This may explain why certain body parts, such as the palms, soles, and areas under the nails, are particularly vulnerable.
Dr. Harb noted that “this type of melanoma frequently develops in areas with less melanin, which provides natural protection against UV damage.”
Dr. Harb contrasted this with the development of superficial spreading melanoma, which frequently appears as a new or changing mole or discoloured area on sun-exposed skin.
The different ways that melanoma manifests in Black and White people emphasizes the significance of thorough skin inspections that include all body parts, not just those that are regularly exposed to the sun.
Research on the prevalence of melanoma in various racial groups is still lacking.
The majority of research papers conducted so far focus on white people’s melanoma cases. Dr. Kamanger noted that as a result, the conclusions that may be drawn are limited by the tiny sample size of Black men.
The primary flaw with this study is that Black men make up less than 0.5% of the population. To obtain useful sub-data, this is a very small quantity, as Dr. Kamanger pointed out.
“The study has some limitations, even if it offers insightful information. It does not take into consideration disease-specific survival, which limits our capacity to distinguish between melanoma mortality and death from other causes,” according to Dr. Harb.
Additionally, certain data were missing, which may have impacted the precision and thoroughness of the findings.
Additionally, compared to white people, there were significantly fewer instances of melanoma among ethnic minority groups. Dr. Harb continued that this can result in bias because the sample might not accurately reflect the entire population.
Taking steps to prevent melanoma
The first step in preventing skin cancer is to shield yourself from the sun. There is no safe level of ultraviolet light exposure, according to Dr. Kamanger, who described ultraviolet light as a real carcinogen.
“UPF clothing, SPF 30 and above sun protection, and seeking shade should be practised.”
Every part of your body, including your feet and nails, should be examined once a month, according to Dr. Kamanger.
When in doubt, schedule a yearly skin cancer test with a board-certified dermatologist, said Dr. Kamanger.
According to Dr. Bubic, “any lesions that may be changing, increasing in size, bleeding, or not healing appropriately should be evaluated.”
REFERENCES:
- https://www.medicalnewstoday.com/articles/melanoma-more-deadly-among-black-men
- https://www.nbcnews.com/news/nbcblk/black-men-are-increased-risk-melanoma-study-finds-rcna93718
- https://www.washingtonpost.com/wellness/2023/07/11/melanoma-skin-cancer-black-men/
For Alzheimer’s disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=10