Lets observe Risky symptoms and complication of Monkeypox.
What Is Monkeypox?
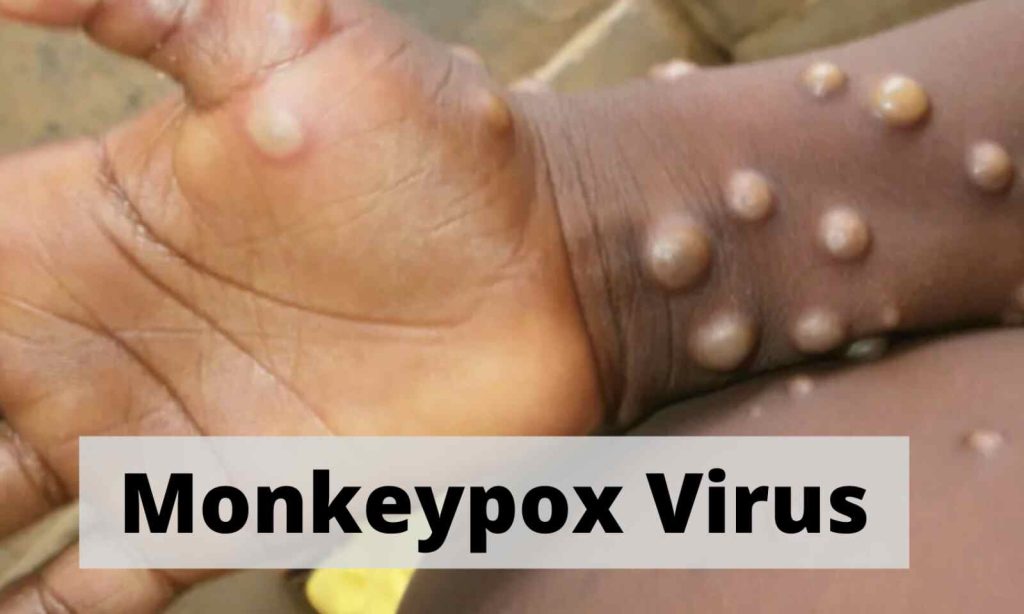
A viral illness called monkey pox is comparable to smallpox. It results in a rash resembling a lesion, lymph node swelling, and fever. Your genitals, anus, and other regions may experience the lesions.
An additional zoonotic disease is monkeypox. This implies that it can spread from animals to people and vice versa. Additionally, it can spread from person to person. The West African virus and the Congo Basin virus are the two forms of monkeypox viruses.
Prior to 2022, central and western Africa was where monkeypox was most prevalent. However, as at the time of this article’s publication, cases of monkeypox brought on by the West African variant of the virus had been reported in 94 countries worldwide, including regions where it is not normally found.
How does the mpox virus spread?
MPX is brought on by the MPX virus. Close contact with an infected animal or person allows the virus to spread. Furthermore, it can spread when someone touches objects, such blankets, that have come into contact with an mpox patient.
People can contract the mpox virus through:
- direct touch with the bodily fluids, scabs, or rashes of a person who has mpox.
- prolonged close proximity to respiratory droplets from an infected person for more than four hours. This covers having sexual relations.
- clothing, bedding, blankets, or other items that have come into contact with an infected person’s body fluids or rashes.
- The mpox virus can infect a pregnant individual and then infect the foetus.
A person contracts mpox from an animal through:
- Bites or scrapes from animals Wild
- cultivated wild wildlife used for food
- Items manufactured from diseased animals
- direct exposure to the bodily fluids or rashes of animals that have the MPOV virus
Where is Mpox found?
The majority of mpox cases for many years were in Africa. It does, however, occasionally appear in other nations, such as the United States. The United States experienced the first mpox outbreak outside of Africa in the spring of 2003. Texas received a consignment from Ghana with diseased animals. The virus was transmitted by the sick rodents to domesticated prairie dogs, which ultimately infected 47 people in the Midwest.
Viruses that were formerly largely confined to certain regions can more easily spread worldwide as international travel becomes more widespread. A case of mpox was discovered in a resident of the United States who had come to the country from Nigeria in the summer of 2021. Then, in 2022, outbreaks spread beyond of Africa to areas in Europe, Australia, and the Americas.
Anyone can purchase mpox. The majority of cases in Africa involve children under the age of 15. The disease appears to be more prevalent in guys who have intercourse with men outside of Africa, although there are many cases in people who don’t fit that description.
Monkeypox symptoms
Monkeypox symptoms are comparable to smallpox symptoms. Typically, monkeypox symptoms are less severe. Symptoms of the monkeypox virus typically take 6 to 13 days to manifest after infection. But it might be anything between 5 and 21 days.
Early warning signs can include:
- The most common first sign is a fever.
- headache
- muscular pain
- back pain
- fatigue
- chills
- Lymphadenopathy, another name for enlarged lymph nodes,
A rash often emerges 1 to 3 days after the fever does. Usually, the rash appears on your:
- face, the most frequent location
- your hands’ palms
- your feet’s soles
- mouth
- genitalia
- the cornea and conjunctiva of the eyes
Before or after a fever and other flu-like symptoms, a rash may appear. Some individuals might only ever have a rash. Lesions that develop in the following order make up the rash brought on by monkeypox:
- flat, brownish blemishes known as macules
- papules, which are mildly elevated lesions
- lumps or vesicles filled with a clear fluid
- lumps or pustules with a yellowish fluid
- scabs
The lesions scab over and fall off once they have healed. Monkeypox symptoms often last 2 to 4 weeks and go away on their own without medical intervention.
Potential complications of monkeypox
The following are potential side effects of monkeypox:
- bronchopneumonia
- sepsis
- Encephalitis, another name for inflammation of the brain,
- inflammation of the cornea, the eye’s transparent outer layer
- further infections
- Loss of eyesight may result from an infection in the cornea.
In extreme circumstances, the lesions may combine. A significant amount of skin loss could result from this.
How is monkeypox treated?
Currently, there is no cure for monkeypox. Monkeypox, on the other hand, has a self-limiting nature and can heal on its own. There are several drugs that can be used to contain an outbreak and stop the illness from spreading. They may consist of:
- Influenza vaccine (smallpox vaccine)
- Immune globulin against vaccinia
- antibiotics for viruses (in animals)
- Smallpox is treated with the antiviral tecovirimat (TPOXX).
- Antiviral brincidofovir (Tembexa), used to treat both adult and child smallpox
Cidofovir, which is normally applied to treat cytomegalovirus-induced eye infections but has also been applied in some instances of monkeypox
With the use of over-the-counter or prescription medications like painkillers, topical creams, and oral antihistamines, other treatments aim to manage symptoms.
REFERENCES:
- https://www.healthline.com/health/monkeypox
- https://www.mayoclinic.org/diseases-conditions/infectious-diseases/expert-answers/monkeypox-faq/faq-20533608
- https://my.clevelandclinic.org/health/diseases/22371-monkeypox
- https://www.cdc.gov/poxvirus/monkeypox/symptoms/index.html
For more details, kindly visit below.