MS severity: Genetic markers may lead to better treatment.
Globally, 2.8 million people will have Multiple Sclerosis (MS) in 2020. The symptoms of MS can worsen over time and result in chronic problems, and the condition presently has no known cure.
The first genetic indicator of MS severity and progression has been identified by researchers at the University of California, San Francisco.
This discovery, according to scientists, may help in the creation of new medications that can delay the advancement of the illness.
Multiple sclerosis (MS), a condition of the central nervous system that affects mobility and vision, will impact roughly 2.8 million individuals worldwide by the year 2020.
MS presently has no known cure. Each person is uniquely affected by the illness, both in terms of when symptoms initially appear and how severe they are.
The severity of the illness can worsen as the body experiences a cycle of symptom flare-ups and remissions, resulting in persistent mobility problems, visual loss, and even partial or complete paralysis.
The first genetic signature connected to MS severity and progression has now been identified by researchers from the University of California, San Francisco.
This discovery, according to scientists, may help in the creation of new medications that can delay the advancement of the illness.
Research targets MS progression
The University of California, San Francisco’s Dr. Sergio Baranzini, professor of neurology and co-senior author of the study, explained that they chose to look for a genetic variation associated with faster MS progression because the disease develops differently in each patient after diagnosis.
“Neurological progression is a common feature in persons with MS, which is inexorable and independent of whether relapses are controlled or not,” he said.
“Some people have a very aggressive disease that can impact their mobility and neurological function in a few years, while others experience a much more benign course,” he said. We already knew that genetics has a significant influence on risk, but the wide range of outcomes revealed that genetics may also affect severity.
Data from The MultipleMS Consortium and The International Multiple Sclerosis Genetics Consortium (IMSGC), two sizable MS research consortiums, were used by Dr. Baranzini and his team.
For a genome-wide association study (GWAS), data from both groups were pooled to represent more than 12,500 MS patients.
From there, researchers combed through more than 7.5 million genetic variants before discovering one linked to accelerated disease progression in MS patients.
This particular mutation is situated between two genes named DYSF and ZNF638 that had no known association with MS. ZNF638 aids in the control of viral infections whereas DYSF aids in the restoration of damaged cells.
Possibility of new treatments for MS
Since there is currently no treatment for MS, doctors employ a variety of drugs to treat the symptoms, delay the disease’s course, and help avoid relapses.
The results of this study, according to Dr. Baranzini, will open the door for a new class of medicines that will treat progression and probably target the central nervous system.
Dr. Baranzini made the point that genetic information considerably reduces the risks associated with drug development because developing medicines represents a considerable risk for the pharmaceutical business, where only a tiny percentage of drugs reach the market.
“This discovery will set up several development programs that will target the unmet need of disease progression in MS,” he said.
“All relapse-controlling medications are immunomodulatory, which is consistent with the genetics of the more than 200 MS risk variations. The central nervous system should be the target of this new class of therapies, according to the genetics of illness severity.”
Dr. Baranzini explained that since it has been proven that genetics contribute to the severity of an illness, the IMSGC is currently preparing for a new genetic study including even more participants.
The researcher continued, “Our prior experience with disease susceptibility suggests that a larger study translates into more findings, and we are pleased to uncover new genetic variants that could aid in the development of more efficient treatments for MS.”
How is MS being treated right now?
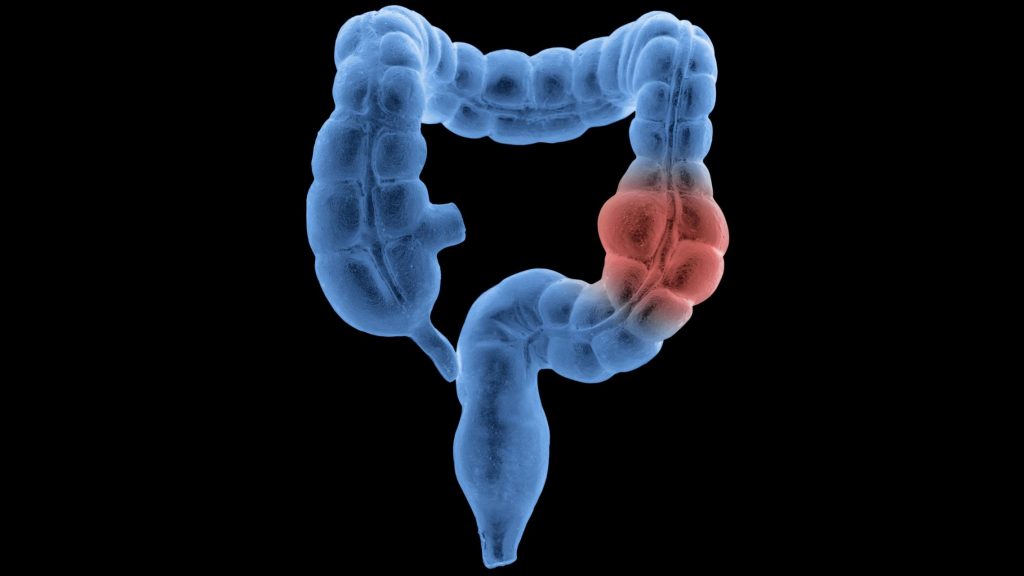
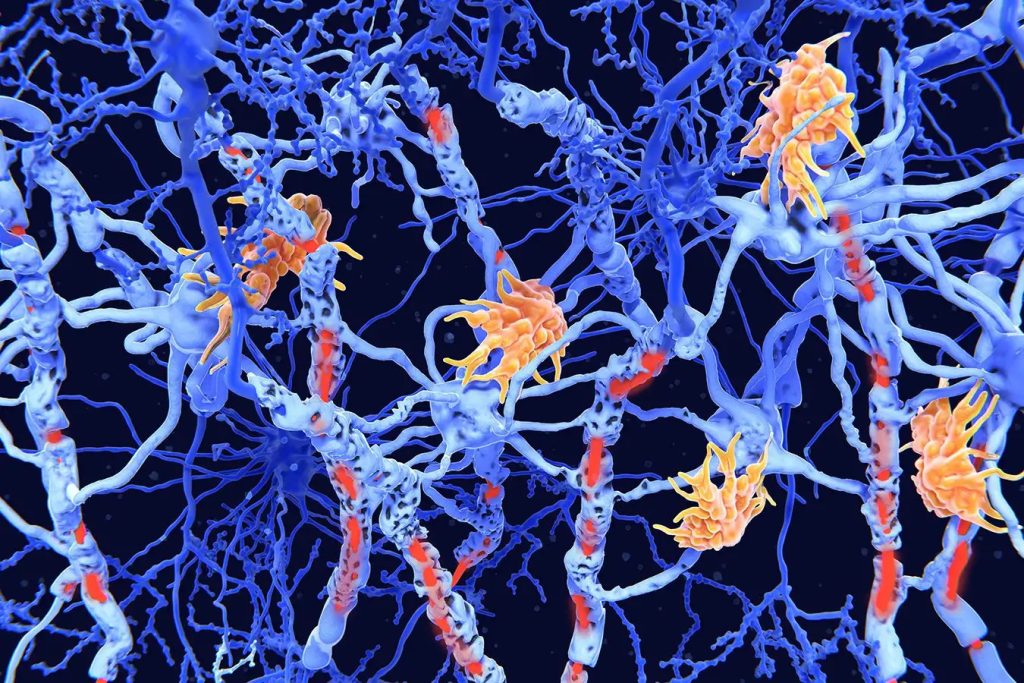
The capacity to move, think, talk, and see clearly can all be significantly impacted by MS since it affects the brain and nerve system.
The majority of scientists concur that MS is caused by the body’s immune system wrongly attacking the central nervous system, even though the exact origin of MS is still unknown.
The myelin that wraps the nerve fibres in the brain and spinal cord is damaged by this onslaught. When myelin is destroyed, it is unable to protect the exposed nerve fibre, which prevents messages from travelling from the nerves to the brain.
Additional MS risk factors include:
- age – between the ages of 20 and 50, most persons acquire a diagnosis
- MS is more prevalent in women than in men.
- an MS family history
- smoking
- a lack of vitamin B12 or vitamin D
- exposure to specific viral illnesses, such as mononucleosis or the Epstein-Barr virus
Why the recent study is beneficial?
We discussed the significance of the study with Dr. Krupa Pandey, director of clinical research at the Neurosciences Institute in New Jersey, director of the Hackensack University Medical Centre MS Centre, and associate professor of neurology at the Hackensack Meridian School of Medicine who was not involved in the current investigation.
She said, “There are a few ways in which this study is helpful. Finding a connection between genes and the potential severity of a disease is a positive step.”
“It is also beneficial since it offers more proof that environmental variables, like smoking, truly do assist people with genetically susceptible diseases to get sicker. This is a fantastic illustration of how a disease may be affected by both nature and upbringing, said Dr. Pandey.
The expert went on to say that similar discoveries “may lead to future findings that can help us counsel patients on how to tailor not just medication regimens but modify lifestyle-related factors.”
“It is also helpful for companies looking at MS therapies [to] enroll patients with higher risks for progression to see if the drug is effective,” she said.
REFERENCES:
- https://www.medicalnewstoday.com/articles/newly-discovered-marker-of-multiple-sclerosis-severity-may-lead-to-better-treatments
- https://www.newscientist.com/article/2380483-genetic-marker-discovered-for-the-severity-of-multiple-sclerosis/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6396336/
- https://www.genengnews.com/topics/translational-medicine/genetic-marker-for-severity-progression-of-multiple-sclerosis-identified/
For Nerve damage medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=30