Can Hormone therapy for menopause increase Dementia risk?
Menopausal hormone therapy is used by about 45% of all women to lessen menopause symptoms.
According to prior studies, some types of hormone replacement treatment may make women more susceptible to developing serious illnesses.
Menopausal hormone therapy is linked to an increased risk of dementia and Alzheimer’s disease, according to researchers from Copenhagen University Hospital, says Rigshospitalet.

These results go against earlier research that suggested HRT might reduce a woman’s risk of dementia.
Menopausal hormone therapy, often known as hormone replacement therapy (HRT), is used by about 45% of all women worldwide to cope with menopause symptoms.
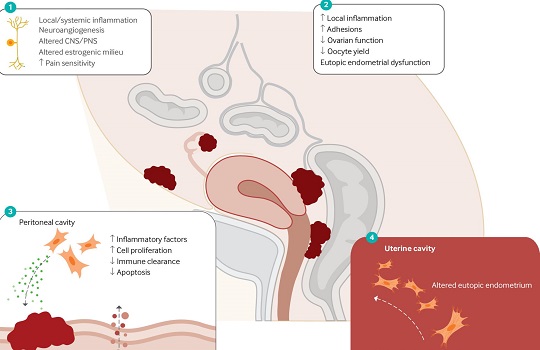
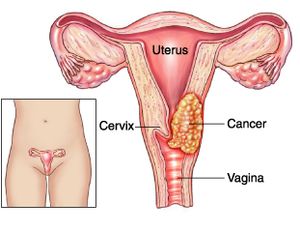
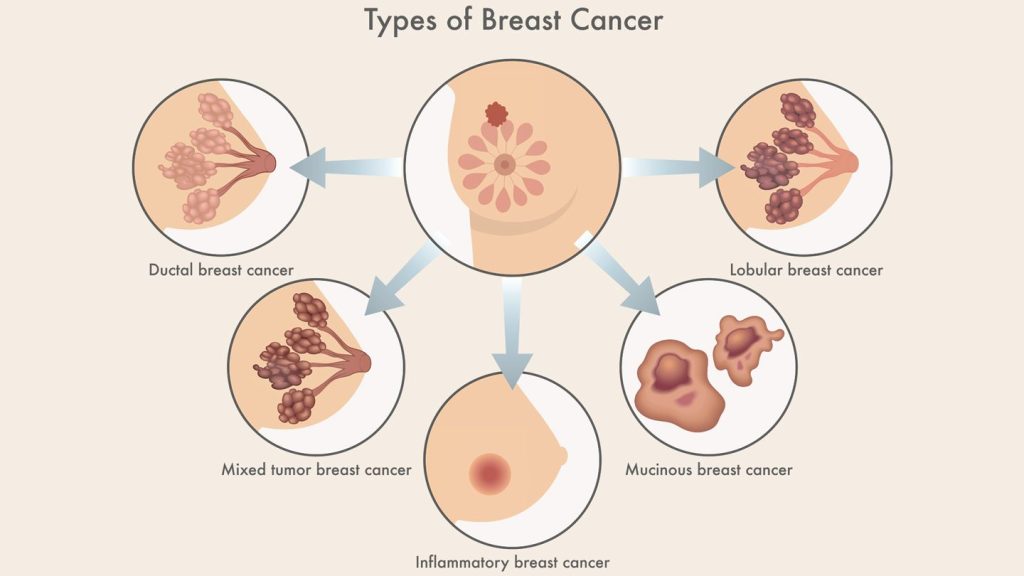
HRT can cause adverse effects like nausea and migraines. According to earlier studies, women who use specific forms of HRT may be more susceptible to strokes, gallbladder problems, and malignancies including breast and endometrial.
Menopausal hormone therapy is now linked to a higher risk of dementia and Alzheimer’s disease, according to study from Copenhagen University Hospital, as per Rigshospitalet.
These results go against earlier research that suggested HRT might reduce a woman’s risk of dementia. The BMJ recently published an article based on this study.
What occurs throughout menopause?
Every woman experiences menopause, which is the end of the monthly cycle and the last time the ovaries release eggs.
Menopause usually begins in a person between the ages of 45 and 55. Perimenopause, often known as the menopausal transition, can persist between seven to fourteen years.
A woman who is beginning menopause may experience symptoms like:
- a hot flash
- morning sweats
- irregular or absent
- vulvar aridity
- difficulty sleeping
- mood swings like anxiousness and depression
Menopause is a natural part of ageing, but it comes with some changes that some people may desire to minimise. Menopause-related symptoms may be treated with the following methods:
- HRT
- hormonal birth control at a low dose
- low-dose mood stabilisers
- prescription or over-the-counter drugs for vaginal dryness
Additionally, several lifestyle modifications can assist in relieving some symptoms:
- routine exercise
- wholesome diet
- meditation techniques
- restricting alcohol
- giving up smoking
- counselling for mood changes
- maintaining a healthy sleep routine
What is hormone therapy for menopause?
The purpose of HRT is to enhance and balance the levels of the female hormones progesterone and oestrogen in the body.
Although the body’s ovaries naturally produce both of these hormones, their production declines after menopause, leading to menopausal symptoms.
There are two primary types of menopausal hormone treatment that a doctor could recommend, depending on a woman’s situation and requirements:
- treatment with just oestrogen
- combined treatment utilising progesterone and oestrogen
HRT can be applied topically or vaginally, and comes in tablet, nasal spray, skin patch, and vaginal cream or suppositories forms.
The following are possible HRT adverse effects:
- bloating
- headaches
- breast discomfort
- nausea
- acne
- mood changes
- uterine bleeding
How Does HRT Affect the Risk of Dementia?
Dr. Nelsan Pourhadi, the study’s lead author and a researcher at the Danish Cancer Society and the Danish Dementia Research Centre in the Department of Neurology at Copenhagen University Hospital – Rigshospitalet in Copenhagen, Denmark, claims that the study’s objectives were dual and based on understudied facets of the subject matter.
“First, we sought to look into whether menopausal hormone therapy use, as advised by guidelines, increased the incidence of dementia.” Second, he told us, “we were looking into continuous versus cyclic therapy regimes.”
Dr. Pourhadi and his team used data from a national registry database for this investigation. The study’s controls were about 56,000 age-matched women without a dementia diagnosis and approximately 5,600 women with dementia. Danish women between the ages of 50 and 60 in 2000 who had no history of dementia or any conditions that would exclude the use of HRT were included in the data, which covered the years 2000 to 2018.
The subjects’ average age at the time of dementia diagnosis was 70. In comparison to controls, 32% of women with dementia and 29% of controls had used estrogen-progestin therapy starting at an average age of 53 before receiving a diagnosis. For dementia-stricken women, therapy lasted an average of 3.8 years, compared to 3.6 years for males.
Analysis revealed that women who got estrogen-progestin therapy had a 24% higher incidence of Alzheimer’s disease and all-cause dementia. Even ladies who started the treatment at age 55 or younger experienced this.
The Women’s Health Initiative Memory Study (WHIMS), the largest clinical experiment in the field, found similar results, according to Dr. Pourhadi.
Does HRT alter the risk of dementia?
Researchers have previously searched for a link between HRT and the risk of dementia.
Menopausal hormone therapy may aid in lowering a woman’s risk of dementia, according to earlier studies. Menopausal hormone therapy use was associated with a lower chance of developing all neurological disorders, including Alzheimer’s disease and dementia, according to a study released in May 2021.
Additionally, a study published in June 2022 discovered that women with depression who used HRT after menopause had a lower risk of developing Alzheimer’s disease and vascular dementia.
Several research have shown a connection between HRT use and an elevated risk of dementia. HRT was linked to a higher incidence of dementia, according to research released in September 2022.
And according to a study that was just released in April 2023, women who had HRT more than five years after the onset of menopause or who started menopause early had greater levels of tau protein in their brains, which is thought to be one of the main causes of Alzheimer’s disease.
When questioned why prior and current studies may have conflicting results, Dr. Pourhadi responded, “It is crucial to emphasise that our findings are in line with those of the largest clinical trial on the topic, WHIMS. The majority of prior clinical trials were hindered by issues like poor selection, limited sample sizes, brief follow-up periods, and results that were purely dependent on cognitive testing rather than a clinical evaluation of dementia.
Furthermore, earlier observational studies, particularly short-term ones, were unable to evaluate the use of menopausal hormone therapy close to menopause, the author continued. The discrepancies between the findings of those studies and those of our study “may be explained by these differences.”
Can HRT lead to dementia?
Dr. Pourhadi explained that because this study is an observational one and not a causal one, it is impossible to establish a link between menopause hormone therapy and dementia.
Therefore, more investigation is required to determine whether or not the observed link may be assumed to be causal. Additionally, it is important to distinguish between the various menopausal hormone therapy delivery methods such as tablets, patches, and gels,” he continued.
Dr. Mindy Pelz, a specialist in holistic medicine who specialises in women’s and hormonal health but was not part in this study, concurred.
It’s vital not to overestimate the results of this new observational study. Correlation does not imply causality, and prior research has shown that menopausal hormone therapy lowers the incidence of dementia, so it’s conceivable there’s a variable missing that we haven’t thought of yet, the researcher added.
She told us that many women go for hormone replacement medication to deal with their symptoms when they have cognitive deficiencies after menopause, which could be a sign of dementia in the future.
Dr. Jewel Kling, assistant director of women’s health internal medicine at the Mayo Clinic in Arizona and a non-participant in this study, informed us after reviewing the findings that because this was an observational study using data from a national registry, we could not draw any conclusions about the cause-and-effect relationship between menopausal hormone therapy and dementia risk.
The only way to conclude causation is through a randomised control design, which this wasn’t. “(We) can only claim that there was a relationship identified between the two in their data. According to the study’s design, there are numerous additional factors that could potentially explain this association, the researcher said.
REFERENCES:
- https://www.medicalnewstoday.com/articles/hormone-therapy-menopause-linked-increased-risk-dementia
- https://www.alzheimers.org.uk/about-dementia/risk-factors-and-prevention/hormones-and-dementia
- https://www.news-medical.net/news/20230703/Study-links-menopausal-hormone-therapy-to-increased-risk-of-dementia-and-Alzheimers.aspx
For Mental disease medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_478