Changes in Cholesterol & triglyceride may affect dementia.
Researchers looked into the impact of varying triglyceride and cholesterol levels on dementia risk.
They discovered that varying amounts of triglycerides and cholesterol raise the incidence of dementia by 19% and 23%, respectively. To comprehend how these results might influence patient treatment, more investigation is required.
Globally, dementia affects around 55 million individuals. This number is anticipated to nearly quadruple to 152 million by 2050 as the world’s population ages.
Strategies for dementia prevention are essential for maintaining health. Finding techniques to mitigate potential risk factors that raise the likelihood of dementia is one way to develop these solutions.
Regular medical care includes tests for triglyceride and cholesterol levels. In order to create hormones and cells, the liver produces a form of fat called cholesterol. A form of fat used for energy is triglycerides.
Clinicians may be able to screen patients for dementia risk and maybe stop or delay the start of the disease by looking at the relationship between blood lipids and dementia risk.
Some evidence suggests a connection between cholesterol fluctuation and dementia. Despite conflicting findings in studies on whether high cholesterol levels increase dementia risk.
Future dementia screening methods and treatments may benefit from a deeper understanding of which lipid components raise dementia risk.
To evaluate whether there is a connection between cholesterol levels and the risk of dementia, researchers recently examined medical records.
“While not necessarily altering practice, this study highlights the need to pay close attention to people with fluctuating cholesterol levels. It will need more research to ascertain if this variance is a real factor in the onset of Alzheimer’s disease or only a side effect of dementia,” said Dr. Dmitriy Nevelev, associate director of cardiology at Staten Island University Hospital and a non-participant in the study.
High risk of dementia associated with fluctuating cholesterol
The average age of the 11, 571 participants the researchers gathered for the study was 71. 54% of the participants were female, and none had ever been diagnosed with Alzheimer’s disease or another type of dementia.
All of the individuals had their blood lipid levels checked for several factors at least three times in the five years before to the study. These comprised:
- cholesterol overall
- triglycerides
- LDL, short for low-density lipoprotein cholesterol
- HDL stands for high-density lipoprotein cholesterol.
Following the participants lasted an average of 12.9 years. 2,473 people experienced the onset of dementia during this time.
Based on how much the individuals’ blood lipid measurements changed, the researchers divided the people into five groups.
In the end, they discovered that those with total cholesterol variability in the highest 20% band had a 19% increased risk of dementia compared to those in the lowest 20%.
Those with triglycerides in the top 20% of the range had a 23% higher risk of dementia than those in the bottom 20%.
The findings persisted after taking into account potential confounding variables like education, initial cholesterol levels, and adherence to lipid-lowering therapies, according to the researchers. They also discovered that changes in HDL and LDL did not correspond to a higher risk of dementia.
Why are changes in lipid levels important?
We discussed how varying triglyceride and cholesterol levels may raise the risk of dementia with Dr. James Giordano, Pellegrino Centre professor of neurology and biochemistry at Georgetown University Medical Centre who was not involved in the study.
He stated that it is unclear whether or how varying cholesterol levels affect the risk of dementia. Nevertheless, he talked about plausible mechanisms from his own study.
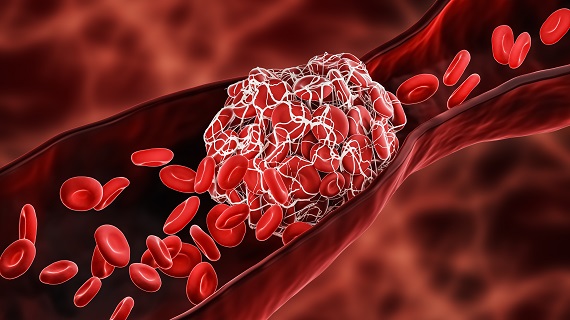
According to Dr. Giordano’s research, “a number of blood-borne factors may cause changes in inflammatory mediators that affect cerebral blood vessels, nerve, and glial cells of the brain cells that remove waste from the brain and deliver nutrients to neurons.”
“This shift to a pro-inflammatory phenotype might interact with existing genetic predispositions in certain individuals. This may increase the risk of several neurodegenerative diseases, including some types of dementia,” he said.
Dr. Nevelev concurred that there is currently no conclusive explanation for why cholesterol fluctuation may raise the risk of dementia.
The functioning of our blood vessel lining is impaired by endothelial dysfunction, which is caused by cholesterol variability. This impairment contributes to irregular blood flow. According to Dr. Nevelev, “Cholesterol variability is also associated with [the] instability of blood vessel plaque, which can likewise obstruct blood flow and harm brain tissue.
He continued, “This study seeks to account for another possibility, which is the effect of sporadic adherence with cholesterol-lowering medicine.
The study did not take into consideration every factor.
We requested an explanation of the study’s main shortcomings from Dr. Howard Pratt, a board-certified psychiatrist and medical director of Community Health of South Florida who was not engaged in the investigation.
“The study’s participants had higher levels of comorbidity than the non-study control group, which did not. Therefore, there can be confounding factors that are harder to identify. Another drawback of the study is that it only included participants from one area, so it’s still not clear whether the conclusions apply to the entire community, the author pointed out.
The apolipoprotein-E (Apo-E) gene, which may have impacted the results of the study, is one genetic risk factor for dementia that was not taken into consideration, according to Dr. Giordano.
Dr. Nevelev was questioned about the study’s constraints as well. He pointed out that it is vital to know whether triglyceride levels were evaluated in samples that were fasting or samples that were not, as triglyceride levels change while a person is fasting.
He continued by saying that variations in body weight are associated with poor health outcomes and that triglyceride and cholesterol levels are related to body weight.
The researcher said, “It is possible that the observation in this study is reversed perhaps those in the early stages of dementia have changes in behaviour or changes in body weight that lead to significant variation in triglyceride levels.”
What effects does this have on preventing dementia?
UTHealth Houston’s McGovern Medical School professor of neurology and director of the Neurocognitive Disorders Centre, Dr. Paul E. Schulz, who was not engaged in the study, said the following to us:
How to apply the findings of this study to the real world is one important question. There are numerous drugs available that lower triglycerides or cholesterol, but I am not aware of any that do the same for fluctuations. Conversely, nutrition has a huge role in managing diabetes. I also wonder if dietary adjustments could also assist lower triglyceride or cholesterol fluctuations, which would lower the risk of dementia.
But given the overwhelming evidence that lower cholesterol is linked to a lower risk of Alzheimer’s disease, he added, “I would still advise people at risk for Alzheimer’s disease to think about taking their statin if their doctor prescribes it to lower their risk for developing Alzheimer’s disease.”
REFERENCES:
- https://www.medicalnewstoday.com/articles/fluctuating-cholesterol-triglyceride-levels-may-influence-dementia-risk
- https://www.news-medical.net/news/20230705/Fluctuating-cholesterol-and-triglyceride-levels-may-increase-risk-of-Alzheimers.aspx
- https://www.webmd.com/alzheimers/news/20230706/dementia-risk-linked-to-cholesterol-fluctuations-study
For Cholesterol medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?therapy=47