Important note on causes and treatment for brain cancer.
The development of malignant cells in the brain leads to brain cancer. Depending on the type of tumour, the cancer cells produce slow- or fast-growing tumours.
The goal of brain cancer treatment is to remove the tumour and then eradicate any cancer cells that may still be present. In particular for slow-growing tumours, new advancements in brain cancer therapies are increasing survival rates.
What is brain cancer?
Primary brain cancer, commonly referred to as brain cancer, is characterised by an excess of brain cells that develops into masses known as brain tumours. Cancer, on the other hand, begins in another place of the body and progresses to the brain. It is referred to as secondary or metastasized brain cancer when that occurs.
Some malignant brain tumours have a rapid rate of growth. These cancerous tumours may interfere with how your body functions. Brain tumours should be treated as soon as they are discovered since they can be fatal.
Brain tumours are rather rare. People have a less than 1% lifetime chance of getting a malignant brain tumour, according to estimates from the American Cancer Society.
Types of brain tumors
Names for brain tumours are determined by their location within the brain or upper spine. A grade is also assigned to tumours. You can determine the projected rate of growth of a tumour by looking at its grade. Grades range from one to four, with four being the fastest-growing grades and one being the slowest.
The following are some of the most prevalent kinds of brain tumours:
- Glioma. About 3 out of 10 occurrences of brain cancer are gliomas, which are brain tumours that start in the glial cells.
- Astrocytoma. Glioblastomas, the kind of quickly-expanding brain tumour, are a subtype of astrocytomas.
- Meningioma. Meningioma tumours, the most prevalent kind of brain tumour in adults, develop in the tissue that surrounds your brain and spinal cord and are frequently benign and slow-growing.
- Ganglioglioma. Surgery is typically used to treat the slow-growing tumours known as gangliogliomas that are present in glial and neuronal cells.
- Craniopharyngiomas. Craniopharyngiomas are slow-growing tumours that develop between the pituitary gland and the brain. Because they frequently encroach on the optic nerves, they can impair eyesight.
- Schwannomas. Almost typically benign, schwannomas are slow-growing tumours that develop around the cranial nerves.
- Medulloblastoma. Children are more likely to develop medulloblastomas, which are rapidly developing tumours that develop on the nerve cells in the brain.
Symptoms of brain cancer
The size and location of the brain tumour affect the symptoms of brain cancer. Particularly in its early stages, brain cancer exhibits many of the same symptoms as a number of less dangerous diseases.
Numerous of these symptoms are extremely typical and are not likely to be signs of brain cancer. However, it’s a good idea to see a doctor if you’ve had any of these symptoms for longer than a week, if they came on suddenly, if they don’t go away with over-the-counter painkillers, or if any of them worry you.
Typical signs of brain cancer include:
- morning headaches that are typically worse
- nausea
- vomiting
- a miscommunication
- a loss of equilibrium
- having trouble walking
- Memory problems
- having trouble thinking
- speech issues
- vision issues
- personality alters
- inconsistent eye motions
- body jerking
- muscle jerking
- unexpected fainting or syncope
- drowsiness
- tingling or numbness in the arms or legs
- seizures
Early diagnosis significantly improves the prognosis for brain cancer. If you frequently suffer any of the aforementioned symptoms or suspect that your symptoms may be more serious, schedule an appointment with a doctor right away for a diagnosis.
Causes and risk factors
Primary brain cancer has an unidentified specific cause. However, studies have connected excessive ionising radiation exposure to a higher chance of developing brain cancer. The most frequent sources of ionising radiation include radiation therapy treatments, frequent medical imaging tests (CT scans and X-rays), and potential employment exposure.
Additional factors that could increase the risk of acquiring brain cancer include:
- greater age
- a history of brain cancer in the family
- chronic smoking
- being exposed to fertilisers, pesticides, and herbicides
- working with substances like lead, plastic, rubber, petroleum, and some textiles that might cause cancer
- having mononucleosis or Epstein-Barr virus infection
Secondary brain cancer Some types of cancer are more likely than others to cause brain cancer, which develops when cancer that started in another part of your body travels to your brain.
The following cancers frequently metastasis, or spread, to the brain:
- lung disease
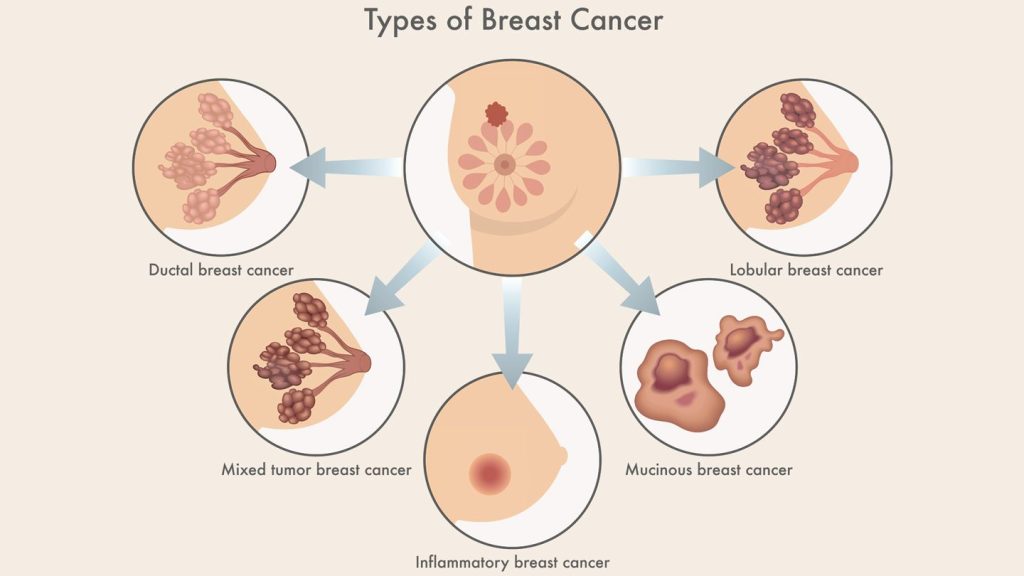
- mammary cancer
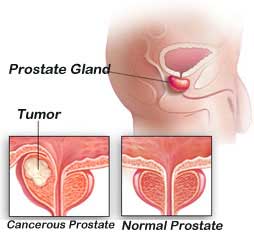
- renal cancer
- urethral cancer
- melanoma, a form of skin cancer
How is brain cancer treated?
Brain cancer can be treated in a number of ways. A primary brain cancer will be treated differently than a cancer that has spread to other organs.
The kind, size, and location of your brain tumour will determine whether you receive one therapy or more. There will also be considerations for your age and general health.
Treatments for brain tumours include:
Surgery.
The most frequent form of treatment for brain tumours is brain surgery. Depending on the tumor’s position, it might be possible to remove it whole, partially, or not at all.
Chemotherapy.
These medications can reduce your tumour and kill brain cancer cells. Chemotherapy can be administered orally or intravenously.
Radiation treatment.
Using high-energy waves like X-rays, this procedure eliminates cancer cells and tumour tissue that can’t be removed surgically.
Combination treatment.
Combination therapy refers to the simultaneous administration of chemotherapy and radiation therapy.
Biologic medicines
These medications support, guide, or restore your body’s natural tumour defences. For instance, immunotherapy is a class of biologic medication that is frequently prescribed and increases your immune system’s capacity to recognise and combat cancer.
Other medicines.
To treat symptoms and adverse effects brought on by your brain tumour and brain cancer therapies, your doctor may prescribe drugs.
Clinical studies.
Clinical trial medicines and drugs may be employed in advanced brain cancer instances that don’t respond to treatment. These are medications that are still being tested. An immunotherapy trial and a CAR T cell therapy trial may be part of clinical trials for brain cancer.
Rehabilitation.
If your disease or treatment have made it difficult for you to speak, walk, or perform other daily tasks, you might need to go to rehabilitation sessions. Physical therapy, occupational therapy, and other types of therapies are all included in rehabilitation. These treatments can assist you in relearnng activities.
Various forms of treatment.
There isn’t much evidence to back up the use of complementary medicines to treat brain cancer. To make up for the nutrients lost during cancer treatment, some medical specialists do advise taking measures like following a bland diet and taking vitamin and mineral supplements.
Before making any dietary changes, using any herbs or supplements, or pursuing any alternative treatments, see your doctor.
How to reduce your risk of brain cancer?
Although there is no known way to prevent brain cancer, you can lower your risk by staying away from:
- pesticide and insecticide exposure
- exposure to cancer-causing substances
- smoking
- radiation exposure that is not essential
REFERENCES:
- https://www.healthline.com/health/brain-cancer
- https://www.cancercenter.com/cancer-types/brain-cancer
- https://www.mayoclinic.org/diseases-conditions/brain-tumor/symptoms-causes/syc-20350084
For more details, kindly visit below.