Lets Explore the types of Cardiomyopathy and its treatment.
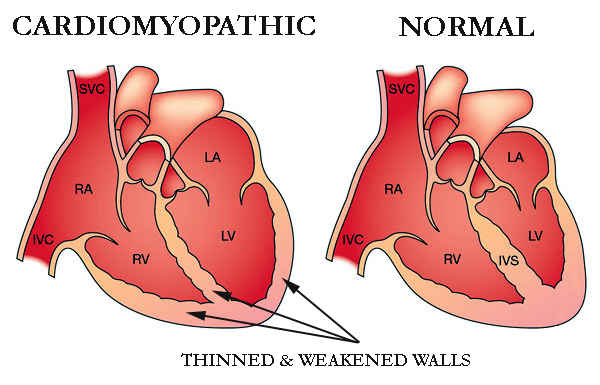
Cardiomyopathy is a condition that affects the heart muscle that gets worse with time and can be fatal. As the heart muscle ages, it becomes less effective in pumping blood.
Cardiomyopathy can be brought on by a genetic trait that is inherited or it can develop as a result of a number of different medical disorders, including heart disease, hyperthyroidism, or alcohol abuse.
Weakness, lightheadedness, shortness of breath, elevated blood pressure, and fluid retention, or edoema, are among the symptoms. Cardiomyopathy can be treated with lifestyle modifications, medicines, and surgery.
Cardiomyopathy is a condition that progressively affects the heart muscle, or myocardium. The heart muscle typically weakens and becomes less capable of properly pumping blood to the rest of the body.
Cardiomyopathy comes in a variety of forms and is brought on by a number of conditions and medications, including coronary heart disease. Heart failure, an irregular pulse, and other consequences can result from cardiomyopathy.
It’s crucial to receive medical care and continue receiving it. They can lessen the risk of heart disease or heart failure.
Types of Cardiomyopathy
Cardiomyopathy comes in a variety of forms, including the following:
Dilated
Heart palpitations and shortness of breath are two symptoms of cardiomyopathy. The most prevalent type of the condition is dilated cardiomyopathy. Adults between the ages of 20 and 60 are the typical victims.
Although the disease frequently begins in the left ventricle, it can later spread to the right ventricle as well. Additionally, the atria’s structure and operation might be impacted by dilated cardiomyopathy.
Hypertrophic
A hereditary disorder known as hypertrophic cardiomyopathy causes the heart muscle fibres to develop abnormally, thickening or “hypertrophying” as a result. The thickening restricts blood flow and stiffens the heart’s chambers. Additionally, it may raise the chance of electrical disturbances, called arrhythmias.
It is the second most prevalent kind of cardiomyopathy in children, according to the Children’s Cardiomyopathy Foundation. Before the age of one year, a diagnosis is made in around one-third of the affected children.
Restrictive
When the tissues in the ventricles stiffen and cannot properly fill with blood, restrictive cardiomyopathy develops. It might eventually result in cardiac failure. It is more prevalent in elderly persons and may be brought on by infiltrative disorders, such as amyloidosis, which involve the buildup of aberrant substances in physiological tissues.
Arrhythmogenic
In arrhythmogenic cardiomyopathy, the healthy tissues of the right ventricle are replaced by fibrotic and fatty tissue, which may lead to irregular heart beats. This procedure may occasionally take place in the left ventricle as well.
Arrhythmogenic cardiomyopathy increases the risk of sudden cardiac mortality, particularly in young individuals and sports, according to study published in the journal Circulation Research. It is a genetic inherited disorder.
Other types of cardiomyopathy
The majority of the following forms of cardiomyopathy fall under one of the previous four categories, however each has different causes or side effects:
Peripartum cardiomyopathy. Cardiomyopathy peripartum can happen before, during, or after pregnancy. This uncommon kind happens in the final month of pregnancy or within five months after delivery when the heart weakens. Postpartum cardiomyopathy is the term sometimes used to describe it after delivery. This dilated cardiomyopathy variant poses a serious risk to life. One instance raises your chances for subsequent pregnancies.
Alcoholic Cardiomyopathy. Alcoholic cardiomyopathy is caused by consuming excessive amounts of alcohol over time, which can weaken your heart and make it less effective at pumping blood. Additionally, your heart may grow. It’s a type of dilated .cardiomyopathy
Ischemic cardiomyopathy. Ischemic cardiomyopathy happens when coronary artery disease prevents your heart from pumping blood to the rest of your body. Heart muscle blood vessels constrict and become clogged. The cardiac muscle cannot receive oxygen as a result. The most common cause of heart failure is ischemic cardiomyopathy. Alternatively, any form of cardiomyopathy that is unrelated to coronary artery disease is referred to as nonischemic cardiomyopathy.
Noncompaction cardiomyopathy. The medical term for this is spongiform cardiomyopathy. It is a rare condition that manifests at birth and is brought on by faulty heart muscle development during pregnancy. Any stage of life may experience a diagnosis.
Pediatric cardiomyopathy. Pediatric cardiomyopathy is the term used to describe cardiomyopathy that affects children.
Idiopathic cardiomyopathy. Idiopathic cardiomyopathy indicates the reason is unknown.
Symptoms of cardiomyopathy
Early on in the development of cardiomyopathy, there may be neither indications nor symptoms. However, when the illness worsens, several indications and symptoms, such as:
- a lack of breath during exercise or even while at rest
- Legs, ankles, and feet swelling
- abdominal bloating brought on by a fluid buildup
- Cough when seated
- difficulty falling asleep flat
- Fatigue
- fast, hammering, or fluttering heartbeats
- chest pressure or discomfort
- Unsteadiness, fainting, and dizziness
If not treated, symptoms and signs frequently worsen. It depends on the individual whether the illness becomes worse swiftly or gradually.
Causes and risk factors
There are certain well-established risk factors for cardiomyopathy, albeit its exact aetiology is not always known. For instance, disorders that cause the heart to inflame or sustain damage can raise a person’s risk of cardiomyopathy.
Cardiomyopathy can also be brought on by heart failure, which can happen as a result of a heart attack or other medical issues.
Additional risk elements consist of:
- a history of cardiomyopathy, sudden cardiac death, or heart illness in the family
- blood pressure is high.
- cardiovascular disease
- The diseases sarcoidosis and amyloidosis, which can harm the heart
- viruses that affect the heart
- diabetes
- drinking disorder
After giving birth, certain women may be at an increased risk for cardiomyopathy.
Research from 2016 indicates, cardiomyopathy risk is also increased by HIV and HIV therapies. Heart failure and dilated cardiomyopathy in particular are risks that are increased by HIV.
Talk to your doctor if you have HIV about obtaining frequent testing to monitor the condition of your heart. Additionally, you ought to make an effort to maintain an active and heart-healthy diet.
Diagnosis of cardiomyopathy
To confirm cardiomyopathy, doctors will do a physical examination and diagnostic procedures. They may employ one or more of the diagnostic tests listed below:
- Chest X-ray: A chest X-ray can assist diagnose some medical disorders by revealing whether the heart has enlarged.
- Electrocardiogram (EKG): A heart’s electrical activity, including how quickly it beats, is measured by an electrocardiogram (EKG). Additionally, it demonstrates if the heart rhythm is normal or irregular.
- Echocardiogram: An echocardiogram produces a moving image of the heart using sound waves. It displays the heart’s size and shape.
- Cardiac catheterization: This procedure examines the blood flow through the heart’s chambers.
How is cardiomyopathy treated?
Treatment for cardiomyopathy focuses on controlling your symptoms. The course of the disease is also slowed by treatment. You will get routine examinations to monitor the condition of your heart.
Your healthcare provider might advise:
Medication: Heart drugs can increase blood flow, address underlying issues, or manage symptoms. You may use beta blockers like propranolol (Inderal), blood thinners like warfarin (Coumadin), or drugs to decrease cholesterol.
Arrhythmia-treating equipment: Pacemakers and implantable cardioverter defibrillators (ICDs) are used to treat erratic heartbeats. Your heartbeat is monitored by these gadgets. When an arrhythmia begins, they send electrical impulses to your heart.
Devices that improve blood flow: Some gadgets make your heart’s blood-pumping process more effective. Devices used in cardiac resynchronization therapy (CRT) regulate the heart’s left and right side contractions. Your heart is assisted in pumping blood with a left ventricular assist device (LVAD).
Surgery: Your doctor might advise heart surgery if you have serious symptoms or underlying heart issues. Open heart surgery or a heart transplant are typically only suggested by healthcare professionals after all other options have failed to provide relief.
REFERENCES:
- https://www.healthline.com/health/heart-disease/cardiomyopathy
- https://www.medicalnewstoday.com/articles/327456
- https://www.mayoclinic.org/diseases-conditions/cardiomyopathy/symptoms-causes/syc-20370709
- https://my.clevelandclinic.org/health/diseases/16841-cardiomyopathy
- https://www.webmd.com/heart-disease/guide/muscle-cardiomyopathy
For more details, kindy visit below.