Cirrhosis: Important causes and symptoms you need to know.
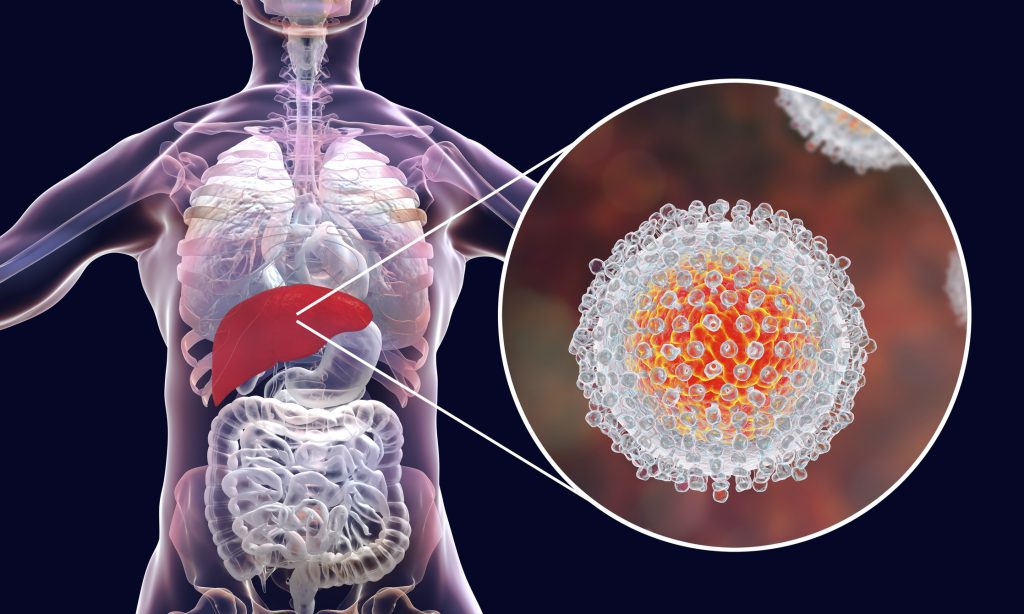
A late-stage liver condition called cirrhosis causes the liver to become irreversibly damaged when good liver tissue is replaced with scar tissue. Your liver cannot function correctly because of scar tissue.

Numerous disorders and diseases of the liver harm healthy liver cells, leading to cell death and inflammation. Cell repair comes next, and the end outcome of the repair process is tissue scarring.
The scar tissue reduces the liver’s capacity to handle nutrients, hormones, medicines, and natural toxins and limits blood flow through the liver (poisons). Additionally, it reduces the liver’s ability to produce proteins and other chemicals. Over time, cirrhosis prevents the liver from functioning normally. Cirrhosis in its advanced stages is fatal.
The stages of cirrhosis
Technically speaking, cirrhosis symptoms can be divided into two stages: compensated cirrhosis and decompensated cirrhosis. It is feasible to transition from the decompensated to the compensated stage if discovered and treated in a timely manner.
- Compensated cirrhosis. The asymptomatic stage is when there are no symptoms present. The liver may still have some scarring, but it hasn’t become severe enough to produce many, if any, symptoms.
- Decompensated cirrhosis. The majority of the symptoms, including ascites and jaundice, manifest during this period. This level is really serious. In certain cases, you may be able to turn your diagnosis back to compensated if you’re able to control the cause of cirrhosis in the first place (for example, heavy drinking).
Symptoms of cirrhosis
At initially, you might not experience any symptoms. However, as time passes and the harm to your liver worsens, you can start to notice:
- Weakness and weary
- Having no appetite and losing weight
- Nausea
Additionally, you can bleed readily, bruise easily, and experience belly or leg swelling. Additionally, you might see modifications in your skin, like:
- Jaundice (when your skin and eyes turn yellow) (when your skin and eyes turn yellow)
- strong itching
- Skin blood vessels that resemble a web of spiders
- Your hands’ palms turning red or your nails turning white
You might have certain mental changes, such as memory or attention issues. It’s possible for women to cease getting their periods. Men may lose their desire for sex, begin to develop breasts, or experience some testicular atrophy.
Other signs you can experience include:
- spitting up blood
- Retention of fluid (swelling in legs, abdominal distension)
- painful muscular spasms
- a brown urine
- Fever
- increased spleen
- bone condition that makes bones more brittle
You might not have all of these symptoms, and some of these issues could also be indicators of other diseases.
Causes and risk of cirrhosis
Always, another liver condition or illness leads to the development of cirrhosis. If the cirrhosis’ underlying cause is not addressed, it will worsen and eventually your healthy liver cells won’t be able to keep up. You can begin to experience fatigue, the urge to skip meals, and unintentional weight loss. Your liver may eventually lose its ability to function well or at all.
Knowing the origin of your cirrhosis is crucial for determining the best course of treatment and preventing further progression. The most frequent reasons include:
- Abuse of alcohol. It’s critical to seek assistance if you have a drinking issue. The liver is harmed by alcohol. Consult your physician. They might suggest a treatment centre for you.
- Fatty liver disease without alcohol. Obesity increases your risk of developing this illness. If this illness is the source of your cirrhosis, losing weight and managing your blood sugar levels may help your liver health.
- Hepatitis B or hepatitis C. The treatment for these illnesses can prevent further liver damage.
The following conditions can also result in cirrhosis:
- Dysplastic fibrosis
- health conditions that make it difficult for your body to metabolise sugar
- Having too much iron in your body
- Wilson’s illness, in which the liver accumulates too much copper
- illnesses that trigger your immune system to assault liver cells
- the bile duct, which transports digestive enzymes from your liver to your intestines, is blocked
- certain gastrointestinal genetic disorders
How cirrhosis is diagnosed?
A thorough history and physical examination are the first steps in cirrhosis diagnosis. A thorough medical history will be taken by your doctor.
If you have a history of chronic alcohol abuse, hepatitis C exposure, autoimmune disease in your family, or any other risk factors, you should be as honest as you can about them.
The physical examination will search for indicators like:
- eyes or skin that appear to be more yellow
- flamboyant palms
- Hand trembling
- an enlarged spleen or liver
- decreased vigilance
The extent of the liver damage can be determined via tests. Among the tests used to assess cirrhosis are:
- an examination of anaemia using a complete blood count
- blood testing for coagulation to determine how rapidly blood clots
- tests for albumin, a protein produced in the liver,
- testing for liver function
- Alpha fetoprotein, a test for liver cancer
The following additional tests can assess the liver:
- an upper endoscopy to check for the presence of esophageal varices
- a liver ultrasound examination
- an abdomen-related MRI
- an abdominal CT scan
- The most accurate test for cirrhosis is a liver biopsy.
Preventing cirrhosis
Hepatitis B or C risk can be decreased by engaging in barrier-method intercourse.
The Centers for Disease Control and Prevention (CDC) advises that all newborns and adults who are at risk, such as medical professionals and first responders, receive the hepatitis B vaccine.
Cirrhosis can be avoided or slowed down by eating a balanced diet, exercising regularly, and limiting or avoiding alcohol consumption. Other preventative strategies comprise:
- Eliminating illicit drugs
- discussing any drugs you take with your doctor, taking them as directed
- getting tested for heptitis if you think you could be susceptible to it
REFERENCES:
- https://www.healthline.com/health/cirrhosis
- https://www.mayoclinic.org/diseases-conditions/cirrhosis/symptoms-causes/syc-20351487
- https://www.medicalnewstoday.com/articles/172295
- https://my.clevelandclinic.org/health/diseases/15572-cirrhosis-of-the-liver
- https://www.webmd.com/digestive-disorders/understanding-cirrhosis-basic-information
For more details, kindly visit below.