Can a daily brief walk could help with depression?
Exercise can enhance brain health, lower disease risk, build bones and muscles, and manage weight.
There is mounting evidence that it can also reduce the signs and symptoms of depression, the main disorder connected to mental health. However, opinions on how much exercise is necessary to have a positive impact vary.
Now, a 10-year research in Ireland has discovered that even little quantities of exercise, like a daily 20-minute stroll, can help older persons experience less despair.

Depression, one of the most prevalent mental health illnesses, is characterized by a persistent sense of emptiness, sadness, or an inability to experience a pleasure. The World Health Organisation (WHO) estimates that it affects about 5% of adults globally.
In 2020, there were 21 million individuals in the United States (8.4% of all adults), and women were more likely than males to experience serious depressive episodes.
According to official government figures, one in six adults in the United Kingdom reported having depressed symptoms in 2021–2022.
Depending on the type of depression a person is dealing with, there are several treatments available, such as antidepressants, psychotherapy like cognitive behavioural therapy (CBT), or a combination of therapy and medicine. Many people find them to be helpful, but once treatment is discontinued, depression may recur.
A little exercise can make a big difference.
There is mounting evidence that altering one’s lifestyle helps lessen depression symptoms. A diet rich in fruit, vegetables, seafood, and whole grains may be linked to a lower incidence of depression, according to a 2014 analysis of 21 research. Additionally, a 2022 analysis of studies revealed that exercise reduced the symptoms of depression.
How much exercise is necessary to reduce depression, however, has not been the subject of many studies.
Now, a ten-year study has discovered that even little exercise helps lessen depression in older persons, defined as those who are 50 years of age and older.
The Health Research Board (HRB) Ireland-funded study, which is published in JAMA Network Open, discovered that a 20-minute brisk walk five times a week dramatically decreased the incidence of depression.
The University of Limerick in Ireland’s Dr. Eamon Laird, the study’s author, explained why the group conducted the investigation:
“Unfortunately, depression is becoming more common in older adults and is linked to a higher risk of developing chronic illnesses like cardiovascular disease (CVD), cognitive decline, death, and suicide. Previous studies have linked physical activity to a lower risk of depression, but no one has ever looked into the absolute minimum amount of physical activity that might be beneficial.
Exercise in general lessens depression
The Irish Longitudinal Study on Ageing (TILDA), a sizable longitudinal study with the goal of enhancing Irish citizens’ ageing experiences, provided the researchers with 4,016 participants. They gathered information between October 2009 and December 2018 at five different intervals.
The researchers used self-completed questionnaires, nurse health assessments, or interviews to gather thorough data on demographic, health, lifestyle, and social aspects at each time point.
The Centre for Epidemiological Studies Depression (CES-D) short form was used to evaluate depressive symptoms. Using this information, they defined major depression as either having a CES-D score more than or equal to nine and/or experiencing a major depressive episode at any moment throughout the data collection process.
Participants self-reported their physical activity over the previous seven days at each data point. They were to keep track of the days they engaged in vigorous, moderate, and walking activities as well as the duration of those activities.
After estimating each person’s weekly total of MET minutes, the researchers divided them into three groups based on their level of physical activity: low, moderate, and high.
Dr. Laird informed us, “We found that older adults who engaged in as little as 20 minutes of moderate to vigorous physical activity (MVPA) per day (for five days a week) had a 16% lower risk of depressive symptoms and a 43% lower odds of depression than those engaging in no exercise.”
The benefits grew as the researchers’ exercise levels rose in each of the three exercise categories. The most active people had a 20% lower chance of developing depression than the least active people.
Even individuals who exercised infrequently had a 16% lower risk of depression than those who did not exercise at all.
Exercise, chronic illness, and depression
Dr. Laird noted that exercise reduced the probability of both depressive symptoms and major depression in people with chronic diseases, and that the benefit grew with increased activity levels.
The WHO standards threshold of 30 minutes a day [per] 5 days [a] week for depressed symptoms was met by participants, specifically for those with chronic conditions, albeit the biggest decreases came with increasing exercise dose, according to the study.
He continued, “In essence, those with chronic diseases may find more benefits. It might be several pathways, including anti-inflammatory, immunological function, heart-brain communication, enhanced muscle performance, etc.”
The study’s non-participant, Dr. Thomas MacLaren, a consultant psychiatrist at Re: Cognition Health, applauded the results.
Chronic health conditions are known to worsen depression and may possibly increase one’s likelihood of getting depressed. The study’s conclusion that there was a dose-dependent association for this group is really positive and shows that adding more brisk walking to your daily routine will help you feel better, he said.
The benefits of exercise for mental health.
Exercise may lower the chance of getting depression or lessen depressive symptoms for a number of reasons.
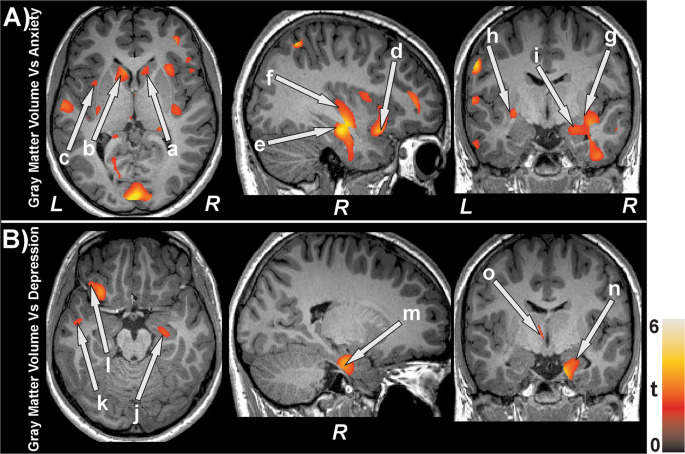
Exercise improves blood flow to the brain, lowers stress reactivity, and stimulates the hypothalamic-pituitary-adrenal (HPA) axis, which affects motivation and mood. Endorphins, the body’s natural pain and stress relievers, are also produced in greater quantities.
As Dr. MacLaren noted, the impacts go beyond the physical.
Exercise raises fitness levels and encourages the body to release endorphins. Your mood can be elevated naturally by these advantageous consequences. Additionally, it may indirectly improve your daily routine and increase social contact, both of which are crucial in the fight against depression.
Dr. Laird concurred, pointing out that for maximum effect, exercise should be a component of a healthy lifestyle.
“Try to incorporate [exercise] into a routine with hobbies or activities that you enjoy, and we would recommend doing it with others as social interactions, particularly with activity, can also have additional benefits for your mental health,” he advised.
“Remember that it is one component and that nutrition and a healthy lifestyle will also give additive benefits in addition to the physical activity,” said Dr. Laird.
REFERENCES:
- https://www.medicalnewstoday.com/articles/just-a-short-walk-each-day-could-reduce-depression
- https://www.apa.org/monitor/2022/11/defeating-depression-naturally
- https://www.eatingwell.com/article/7960746/walking-reduce-depression-risk-new-research/
For Depression medications that have been suggested by doctors worldwide are available here https://mygenericpharmacy.com/index.php?cPath=77_478