How dangerous is Retinoblastoma for babies and toddlers?
The retina is where Retinoblastoma, an eye cancer, first appears (the light-sensitive tissue at the back of your eye). Children younger than five are most frequently affected by it. Adults and older children can occasionally contract it as well.
Even though retinoblastoma is the most frequent cancer in children, it is still uncommon. Only 200 to 300 kids are diagnosed with retinoblastoma annually in the United States. It affects both males and girls equally, regardless of race or ethnicity. One or both eyes may develop retinoblastoma.
Early detection of this eye cancer is crucial because it is frequently treatable.
What is retinoblastoma?
The thin layer of light-sensitive tissue that lines the back of your eye is called the retina. It is in charge of absorbing light, converting it into neural impulses, and transmitting these signals as images to your brain.

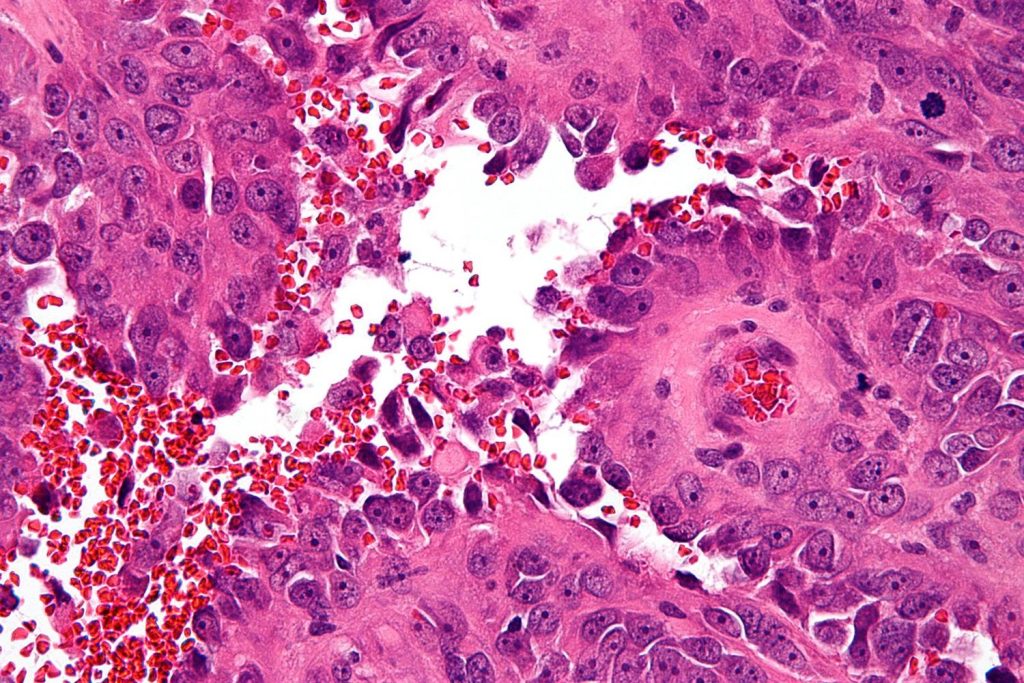
Retinoblasts are cells that develop into the retina’s nerve cells throughout development. Retinoblastoma can develop if some of these cells proliferate uncontrollably. When the nerve cells (neurons) that form the retina have genetic alterations, retinoblastoma develops.
Retinal neurons divide and grow very quickly in the early stages of a child’s development until they eventually halt. These genetic abnormalities cause retinal neurons to proliferate and divide uncontrollably in children, leading to the development of tumours.
Young children are most at risk for having retinoblastoma because their neurons develop so quickly. In actuality, retinoblastoma typically affects children under the age of 6 and is diagnosed at an average age of 2 in those who do.
How does retinoblastoma develop?
Long before birth, the development of the eyes begins. Retinoblasts are cells that exist in the early stages of eye development and replicate to produce new retinal cells. These cells eventually cease proliferating and develop into mature retinal cells.
It happens very infrequently for this process to go awry. Some retinoblasts don’t mature; instead, they grow uncontrollably and develop into the malignancy retinoblastoma.
Retinoblastoma is caused by a complicated series of cellular events, but it virtually invariably begins with a change (mutation) in the RB1 gene. A mutation in the RB1 gene prevents it from functioning as it should, despite the fact that the normal RB1 gene aids in preventing uncontrolled cell growth. There are two main forms of retinoblastomas that can develop depending on where and when the RB1 gene is altered.
What causes retinoblastoma?
Retinoblastoma comes in two varieties: inheritable and sporadic. They stem from several causes. Let’s examine each in greater depth.
Inherited Retinoblastoma
Approximately one-third of all cases of retinoblastoma are inherited. In this type, not just a child’s retinal cells but every cell in their body has cancerous abnormalities.
The majority of the time, these mutations are acquired relatively early in a child’s development, but occasionally, they are passed down from one of the parents. The two eyes are most frequently affected by this kind of retinoblastoma (bilateral retinoblastoma).
There is a possibility that you will convey the retinoblastoma-causing gene to your offspring if you carry it. Because of this, it’s crucial to consult a genetic counsellor if you have ever received a diagnosis for this ailment and intend to become a parent.
Sporadic Retinoblastoma
A child will not have retinoblastoma mutations in every cell in their body in the remaining two-thirds of retinoblastoma cases. Instead, one retinal neuron in one of their eyes experiences a mutation that causes it to divide uncontrollably, which is when their cancer initially manifests.
You cannot pass sporadic retinoblastoma on to your offspring. It’s unclear what causes the genetic changes that lead to retinoblastoma in children, whether it’s inheritable or sporadic. It’s crucial to keep in mind that there are no recognised risk factors for this illness, thus there was nothing you could have done to stop the condition from afflicting your child.
A youngster must, however, undergo early screening if there is a family history of retinoblastoma.
Symptoms of Retinoblastoma
Retinoblastoma typically affects infants and young children, therefore its symptoms aren’t always immediately noticeable. You might spot some of the following symptoms in your child:
- Instead of the traditional red reflex, leukocoria, a white reaction that develops as light enters the pupil, or a white mass behind one or both pupils that is frequently observed when a flash shot is taken
- Eyes that strabismus, or gaze in various directions (crossed eyes)
- redness and swollen eyes
- Nystagmus, or uncontrollable, repetitive eye movements
- bad vision
Other symptoms are possible, but they are often less prevalent. Make an appointment with your child’s paediatrician if you see any of these signs or any other changes in one or both of your child’s eyes that worry you.
How is retinoblastoma treated?
Each patient’s retinoblastoma treatment is unique. It relies on a number of variables, such as:
- the tumor’s size
- the tumor’s location
- whether only one eye is impacted or both
- stage of the tumour and whether it has migrated to tissues away from the eye (metastasis)
- age and general well-being
Retinoblastoma treatments include:
- chemotherapy
- Cryotherapy, sometimes called cold therapy
- laser treatment
- radiation treatment
- Enucleation, or the removal of the afflicted eye via surgery
To get the best outcomes, doctors occasionally combine various therapies.
Treatment for retinoblastoma that only affects one eye relies on whether the eye’s vision can be preserved. If the tumour affects both eyes, surgeons will attempt to preserve some vision by saving at least one eye.
The objectives of treatment for retinoblastoma are:
- to preserve the kid’s life
- eradicate cancer
- to try and keep the eye
- keeping as much of the vision as feasible
to reduce the chance of treatment adverse effects, particularly radiation therapy, as it could raise the likelihood that a kid would later get another form of cancer.
REFERENCES:
- https://www.healthline.com/health/cancer/retinoblastoma
- https://www.mayoclinic.org/diseases-conditions/retinoblastoma/symptoms-causes/syc-20351008
- https://www.webmd.com/cancer/what-is-retinoblastoma
- https://www.cancer.org/cancer/retinoblastoma/about/what-is-retinoblastoma.html
- https://my.clevelandclinic.org/health/diseases/10706-retinoblastoma-cancer-of-the-eye
For more details, kindly visit below.