Critical reasons you need to know about Gonorrhea.
What is gonorrhea?
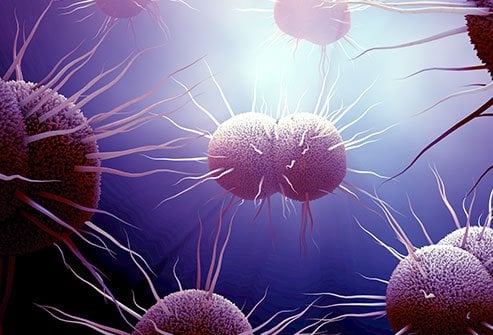
A bacterium called Neisseria gonorrhoeae is the prevalent sexually transmitted infection (STI) known as gonorrhoea (N. gonorrhoeae). Additionally, it goes by the names “the clap” and “drip.” Semen and vaginal fluid are two sexual fluids that can spread gonorrhoea. Intercourse, anal sex, oral sex, and sharing sex toys with an infected person are all ways to contract gonorrhoea.
Gonorrhea frequently has no symptoms. This makes it simple to unintentionally infect your companions. You can lower your risk of infection by getting tested periodically, as advised by your healthcare professional, and using safer sex techniques.
How is gonorrhea transmitted?
Having vaginal, anal, or oral intercourse can result in gonorrhoea transmission or infection. When having intercourse, using a condom or another barrier device can significantly reduce your risk of developing or spreading STIs like gonorrhoea.
Just bear in mind that, especially if you misuse these barrier measures, they may not always entirely reduce your risk. Here’s how to properly use barrier devices and condoms.
According to some data, French kissing, or kissing with the tongue, may also be a means of transmission for oral gonorrhoea. To fully grasp the potential risk of transmission, more research is necessary.
You are more likely to get gonorrhoea again if you have once had it. Gonorrhea left untreated can raise your chance of acquiring more STIs. During delivery, gonorrhoea can potentially be passed from the mother to the child.
Symptoms of Gonorrhea
Many gonorrhoea sufferers show no signs of the disease. People who do frequently have a burning feeling while urinating.
Additionally, a man with a penis might see:
- discharge that is white, green, or yellow.
- swelling or discomfort in the testicles
- Foreskin irritation or edoema
- Increased vaginal discharge and bleeding between periods are possible in vaginal patients.
If someone has anal sex, they may also experience rectal problems. These may consist of:
- discharge
- scratching at the anus
- soreness
- bleeding
- Having bowel motions hurt
Oral intercourse can induce gonorrhoea, which can be found in the throat but may not show any symptoms. Because gonorrhoea is a bacterial illness, conjunctivitis, a common eye condition, could result from semen or vaginal fluid containing the bacterium.
What causes gonorrhea?
When the gonorrhea-causing bacteria (N. gonorrhoeae) enters your body through sexual fluids like semen or vaginal fluid—often through unprotected sex—you get an illness. Your mouth, vagina, penis, or anus are all possible entry points for the germs. To transfer the bacterium, neither you nor your partner need to ejaculate (cum). Sharing sex accessories that haven’t been cleaned or wrapped with a fresh condom can potentially spread gonorrhoea.
The cervix is the most typical site of infection in those who are born with the gender given to them. Your uterus and vagina are connected by a passageway called the cervix.
Infection commonly begins in the urethra, the tube through which urine leaves the body, in those who were born with the gender ascribed to them as male.
Who gets gonorrhea?
Gonorrhea can be contracted by sexually active individuals of any age or sex and passed on to partners. When you give birth, you could infect your child.
You’re more likely to contract an infection if you:
- are under 25.
- have a STI history.
- Never use dental dams or condoms every time you have intercourse.
- are engaging in sexual activity with one or more partners who have not had gonorrhoea tested.
- Are a man or woman with a penis who engages in sexual activity with other men or women with penises (MSM).
Complications of gonorrhea
You are more likely to have long-term gonorrhea-related issues if you have a vagina.
Gonorrhea and chlamydia are two STIs that can spread into the reproductive system and harm the uterus, fallopian tubes, and ovaries if left untreated. This may result in pelvic inflammatory disease, a disorder (PID). PID can harm the reproductive organs and result in excruciating, ongoing agony.
Another potential problem is fallopian tube blockage or scarring, which can:
- make getting pregnant more challenging
- cause ectopic pregnancy, which occurs when an egg that has been fertilised implants outside the uterus.
During delivery, gonorrhoea can potentially spread to a newborn child. Gonorrhea, if left untreated, can result in: if you have a penis.
- Urinary tract scarring
- a distressing penile abscess that could have an impact on your fertility
- Inflammation of the semen-carrying tubes close to your testicles is known as epididymitis.
- Untreated infections can also enter your bloodstream, where they might result in uncommon but severe side effects like arthritis and heart valve damage.
REFERENCES:
- https://www.mayoclinic.org/diseases-conditions/gonorrhea/symptoms-causes/syc-20351774
- https://www.healthline.com/health/gonorrhea
- https://my.clevelandclinic.org/health/diseases/4217-gonorrhea
- https://www.medicalnewstoday.com/articles/155653
For more details, kindly visit below.
