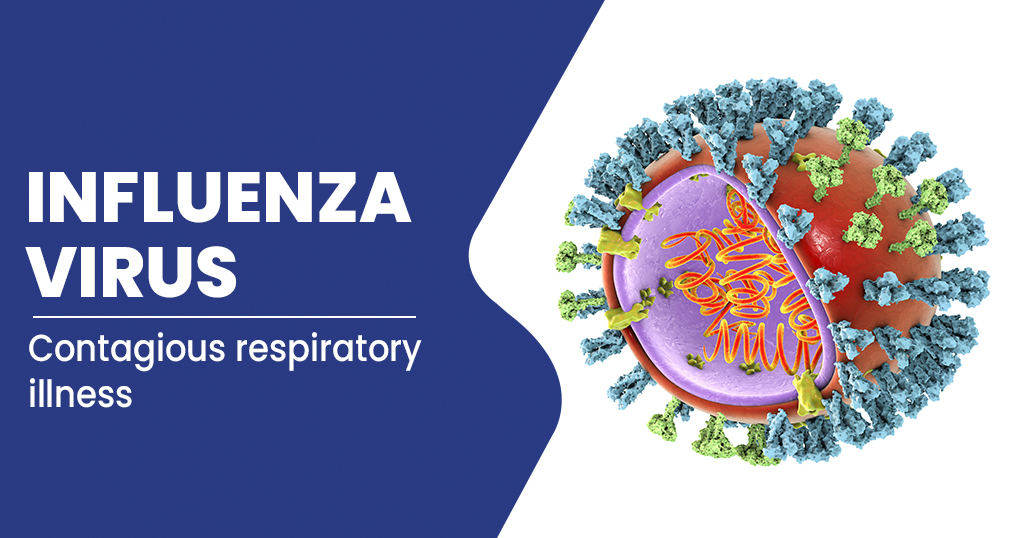
Bird flu: Risks and complication you need to know.
Avian influenza, commonly known as bird flu, is a virus that can infect not just birds but also people and other animals. The majority of the virus’s variants only affect birds.
The most prevalent strain of avian flu is H5N1. It can easily infect people and other animals who come into touch with a carrier and is fatal to birds. The World Health Organization reports that since H5N1 was initially identified in humans in 1997, over 60% of people who contracted the disease have died.

The virus is not known to pass from person to person at this time. However, some specialists are concerned that H5N1 could eventually threaten humans with a pandemic.
Health officials are concerned that if a bird flu virus mutates into a version that spreads more quickly from person to person, a global outbreak might happen. The development of vaccinations to help prevent the spread of avian flu is now underway.
How avian influenza virus is spread?
All avian influenza type A viruses are thought to be carried by water birds, such as wild ducks. Bird faeces act as a vehicle for the viruses to leave the bird’s intestines and enter the environment (poo). Bird flu might potentially spread from diseased migratory birds to any nation they travel to.
Wild birds don’t typically exhibit bird flu symptoms, but the H5N1 virus that is presently circulating has made some wild birds sick and even killed them. Domesticated species, including chickens and turkeys, are more frequently killed by the avian influenza virus.
The signs that can appear in birds vary depending on the species, but they can include vomiting, trouble breathing, a swelled head, and even death. The virus is excreted by ill birds in their feathers, mucus, saliva, and faeces.
Bird flu can infect people who come into close contact with sick birds. For instance, a person might touch a sick bird, get chicken faeces on their hands, and neglect to wash their hands before eating. The infected bird poop will subsequently be consumed by them. The most typical route for a human to contract avian flu is through this. Although it can persist in raw poultry flesh as well, the virus is killed by conventional cooking.
There is no proof that the H5N1 avian flu variant that is now circulating can be easily transmitted from person to person.
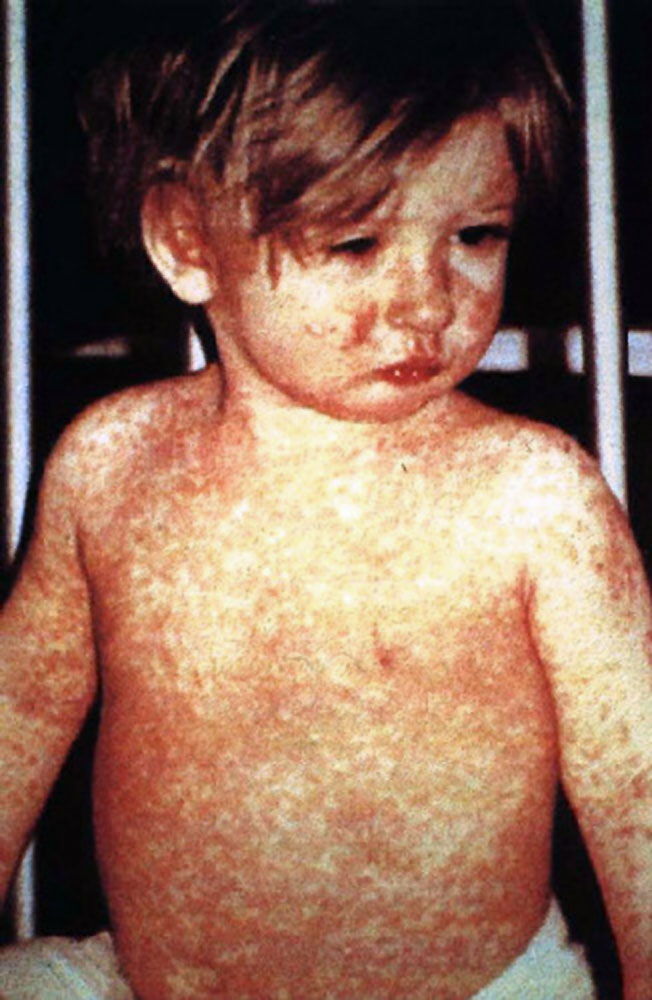
Symptoms of bird flu
If you suffer symptoms similar to the flu that are more severe than those of the flu, such as:
- cough
- diarrhoea
- respiratory problems
- fever (over 38°C or 100.4°F)
- headache
- muscular pain
- malaise
- clogged nose
- unwell throat
Before you visit the doctor or hospital, you should let the personnel know if you have been exposed to the bird flu. By letting them know beforehand, they can take preventative measures to safeguard personnel and other patients before taking care of you.
What causes bird flu?
Despite the fact that there are other strains of bird flu, H5N1 was the first to infect people. In 1997, the first infection took place in Hong Kong. The handling of diseased chickens was connected to the outbreak.
Although H5N1 normally exists among wild waterfowl, it can spread quickly to farmed poultry. Humans can contract the disease by coming into contact with contaminated bird excrement, nasal secretions, or eye or mouth secretions.
The bird flu cannot be contracted by eating properly cooked poultry or eggs from sick birds, however runny eggs should never be served. When meat reaches an internal temperature of 165°F (73.9°C), it is deemed safe.
Bird flu risk factors
H5N1 has the capacity to endure for long stretches of time. For up to 10 days, H5N1-infected birds continue to expel the virus in their faeces and saliva. The infection can spread by touching infected surfaces.
You may be more susceptible to getting H5N1 if you are:
- a farmer of poultry
- a visitor to the impacted areas
- being exposed to diseased birds
- one who consumes raw poultry or eggs
- a medical professional treating infected individuals
- a member of the sick person’s family
Complications of Bird flu
When afflicted with the avian flu, a person may experience serious health issues, such as:
- Pneumonia
- Red eye (conjunctivitis)
- respiration difficulty
- a kidney problem
- Heart issues
Because so few people have contracted bird flu, even though it may kill more than half of those it infects, the number of fatalities is still modest. Since 1997, the World Health Organization has received reports of fewer than 500 bird flu fatalities.
The seasonal flu, on the other hand, is thought to be the sole cause of thousands of deaths annually in the United States, according to the Centers for Disease Control and Prevention.
REFERENCES:
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/bird-flu-avian-influenza
- https://www.healthline.com/health/avian-influenza
- https://www.mayoclinic.org/diseases-conditions/bird-flu/symptoms-causes/syc-20368455
- https://www.britannica.com/science/bird-flu
For more details, kindly visit below.