Characteristics of peptic ulcers and its complications.
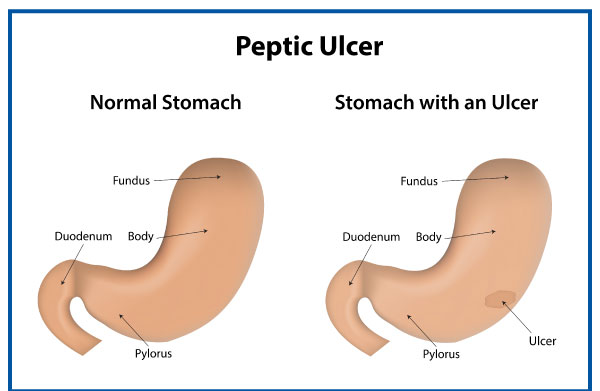
What are peptic ulcers?
If you have open sores in your stomach or upper small intestine, you may have a peptic ulcer. That occurs when the mucus lining your digestive tract’s protective layer is removed by stomach acids. There can be no symptoms, or there might be discomfort or a sharp ache. Internal bleeding brought on by peptic ulcers can occasionally need receiving blood transfusions in a medical facility.
Researchers predict that 8.09% of people worldwide experienced at least one peptic ulcer in 2019; which is a 25% increase since 1990. According to the same study, fewer occurrences have been documented in the US since the first half of the 20th century. Between 1990 and 2019, they started to rise once more.
Peptic ulcers come in three different varieties:
- Internal stomach ulcers are referred to as gastric ulcers.
- Esophageal ulcers are so named because they appear inside the oesophagus.
- Duodenal ulcers are ulcers that form in the duodenum, the upper portion of the small intestine.
Symptoms of peptic ulcers
Peptic ulcers may not show any symptoms at all or they may just produce minor discomfort. Others can feel a stomach ache that is both dull and searing.
Additional signs can include:
Ulcers can result in severe symptoms, bleeding, and indications. These are symptoms of an ulcer that is bleeding:
- throwing up blood
- faeces that are dark crimson in colour or that are black and tarry
- nausea and vomiting that is particularly intense and continuous
A medical emergency is indicated by these symptoms. The patient has to see a doctor right away or dial 911.
Causes of peptic ulcers
There are numerous potential causes of peptic ulcers, however the two most frequent ones are as follows:
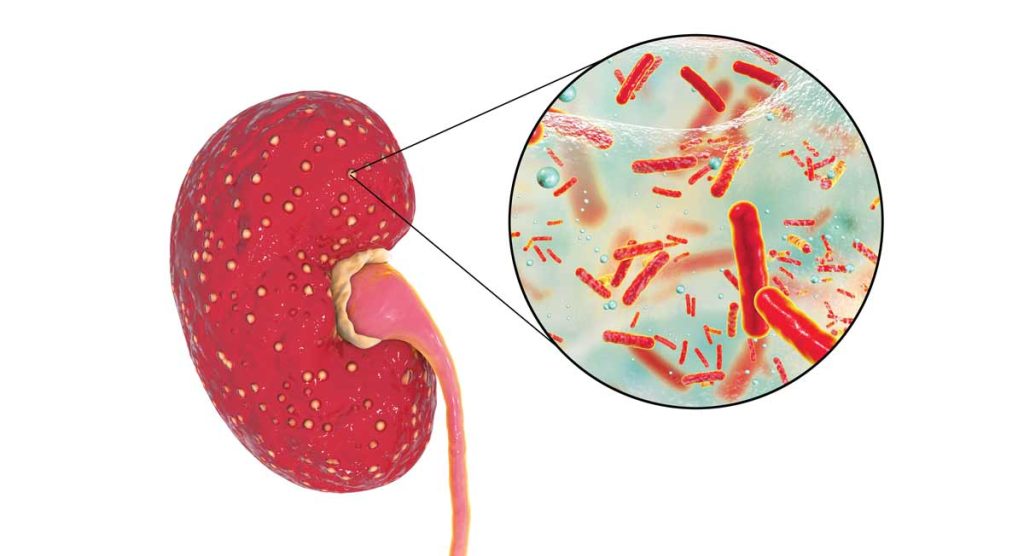
H. pylori cause ulcers
It is unclear why H. pylori bacteria only cause ulcers in some people, despite the fact that many people naturally carry them. H. pylori spread via water and food. They reside in the mucus that covers the lining of the stomach and duodenum and generate the enzyme urease, which reduces the acidity of stomach acid, neutralising it.
The stomach creates more acid to make up for this, which irritates the stomach lining. Additionally, the germs irritate the stomach and impair its immune system.
Nonsteroidal anti-inflammatory drugs cause ulcers
NSAIDS are a class of drugs frequently used for headaches, menstrual cramps, and other symptoms. They can also aid in lowering inflammation and fever. Ibuprofen and aspirin are two examples. Many NSAIDs are accessible over-the-counter.
They lessen the stomach’s capacity to produce a thick layer of mucus for protection. As a result, stomach acid has a greater potential to harm Trusted Source. NSAIDs may also hinder blood flow to the stomach, which would hinder the body’s capacity to repair cells.
Other causes of peptic ulcers
Among the additional probable causes of peptic ulcers are:
- Genetics: Many people who have peptic ulcers have relatives who also have the condition, indicating that hereditary factors could be at play.
- Smoking: It’s possible that people who smoke tobacco frequently have a higher risk of developing peptic ulcers than people who don’t smoke, though it’s unknown how smoking affects peptic ulcers specifically.
- Alcohol consumption: Alcohol consumption can aggravate the lining of the stomach and raise acidity.
- Use of corticosteroids: Studies have shown that those who use high or ongoing dosages of corticosteroids are also at higher risk.
Studies on the link between stress and an increased risk of ulcers are contradictory, but one study revealed that psychological stress may make peptic ulcers more common in a way that cannot be explained by other factors like NSAID use.
Complications of a peptic ulcer
Ulcers that are left untreated may worsen over time. They may trigger additional, more severe health issues like:
- Perforation: An infection results from a hole that forms in the stomach or small intestine lining. A perforated ulcer can cause abrupt, excruciating stomach pain.
- Internal bleeding: Because bleeding ulcers can cause severe blood loss, hospitalisation is often necessary. Lightheadedness, wooziness, and dark stools are symptoms of a bleeding ulcer.
- Scar tissue: After an accident, thick tissue known as scar tissue forms. Food has a tough time moving through your digestive tract because of this tissue. Vomiting and weight loss are indications that there is scar tissue.
All three issues are significant and might necessitate surgery. If you suffer any of the following symptoms, get emergency medical help right away:
- unexpectedly acute abdominal ache
- extreme perspiration, fainting, or confusion, as these could be symptoms of shock
- blood in the stool or vomit
- a difficult-to-touch abdomen
- stomach ache that gets better when lying perfectly motionless but gets worse when you move around
Diagnosis of peptic ulcers
During a regular exam, a doctor will frequently become suspicious of a peptic ulcer due to a patient’s description of their symptoms.
The following tests can support a diagnosis:
- an H. pylori blood test, while a positive result does not usually indicate a current infection
- a breath test that detects H. pylori using a radioactive carbon atom.
- a stool antigen examination to find H. pylori in the stools
- using a GI (upper gastrointestinal) X-ray) to look for ulcers
The most popular device used by doctors to make diagnoses is Upper endoscopy or esophagogastroduodenoscopy. In order to check for the presence of an ulcer in the stomach and upper intestine, a tube must be inserted through the mouth.
The doctor may take a biopsy (a small sample of tissue) to be examined under a microscope if the test reveals an ulcer. A biopsy can check for cancerous tissue and test for H. pylori. A second endoscopy may be required a few months later to check on the ulcer’s progress.
Treatment of peptic ulcers
The goal of treatment will be to either completely eradicate the H. pylori infection or reduce stomach acid levels to allow the ulcer to heal. The following are typical treatments that a doctor might suggest:
- Antisecretory substances. To help reduce the production of stomach acid, these include proton pump inhibitors and H2 receptor antagonists.
- Triple treatment. To get rid of H. pylori, two antibiotics plus a proton pump inhibitor are used.
- Staying away from NSAIDs. If someone regularly uses NSAIDs, doctors advise against using them.
- Surgery. A doctor may advise surgery in cases of bleeding, with an average recovery time of 8 to 12 weeks.
REFERENCES:
- https://www.medicalnewstoday.com/articles/9273
- https://www.healthline.com/health/peptic-ulcer
- https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc-20354223
- https://my.clevelandclinic.org/health/diseases/10350-peptic-ulcer-disease
- https://www.webmd.com/digestive-disorders/peptic-ulcer-overview
For more details, kindly visit below.