Lets gaze upon important Hernia types and their risks.
What is Hernia?
When an organ pulls through a tear in the muscle or tissue holding it in place, a hernia results. For instance, a weak spot in the abdominal wall may be breached by the intestines.
Hernias are common in the area of your abdomen between your chest and hips, but they can also develop in the region of your upper thighs and groyne.
While most hernias don’t pose a life-threatening hazard right away, they also don’t go away on their own. Surgery may occasionally be necessary to avoid potentially serious side effects.
Types of hernia
Hernias come in many different forms. We’ll look at a few of the more popular ones below.
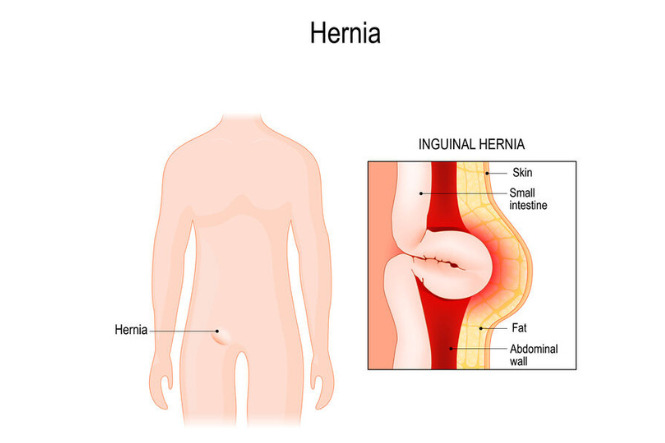
Inguinal hernia
The most typical kind of hernias are inguinal hernias. They take place when a weak area or rip in the lower abdominal wall, frequently in the inguinal canal, is breached by the intestines.
Your groyne contains the inguinal canal. It is the region in men where the spermatic cord connects the scrotum to the abdomen. The testicles are where this rope fastens. The round ligament, which is found in the inguinal canal in females, aids in holding the uterus in place.
Because the testicles descend through the inguinal canal soon after birth, inguinal hernias are more common in men. Behind them, the canal is planned to almost entirely close. Occasionally, the canal won’t completely shut, creating a weak spot. Study up on inguinal hernias.
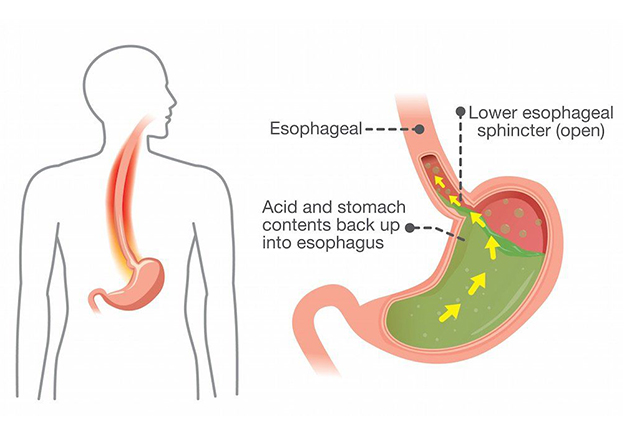
Hiatal hernia
When a portion of your stomach pushes through the diaphragm and into your chest cavity, it is known as a hiatal hernia. The diaphragm is a muscular sheet that contracts to bring air into the lungs, aiding in breathing. It divides the organs in your chest from those in your abdomen.
The majority of cases of this kind of hernia occur in adults over 50. If a child has the syndrome, a congenital birth defect is often to blame.
Gastroesophageal reflux disease is usually always brought on by hiatal hernias (GERD). The stomach’s contents seep backward into the oesophagus in GERD, giving the patient a burning feeling. Find out more about hiatal hernias.
Umbilical hernia
Children and infants may experience umbilical hernias. When the intestines protrude through the abdominal wall close to the belly button, they develop. If your child is weeping, you might see a bulge in or close to their belly button.
Only an umbilical hernia frequently resolves by itself when the muscles of the abdominal wall get stronger. By the time the child is 1 or 2 years old, this usually occurs. dependable source If the hernia has not disappeared by the time the child is five years old, surgery can be done to treat it.
Umbilical hernias can also occur in grownups. They can develop as a result of the abdomen being repeatedly strained by situations including obesity, ascites, or pregnancy. Learn more information about umbilical hernias.
Hernia ventral
When tissue protrudes via a tear in the muscles of your abdomen, it is known as a ventral hernia. When you’re lying down, a ventral hernia could seem to get smaller.
A ventral hernia can occur from birth, but it’s more likely to develop throughout the course of your lifetime. Obesity, pregnancy, and intense activity are all common causes of ventral hernias.
A surgical incision site can also experience ventral hernias. An incisional hernia can develop as a result of abdominal muscular weakening near the surgery site or surgical scarring.
Causes of Hernia
A hernia typically has no evident cause, with the exception of an incisional hernia (a side effect of abdominal surgery). Hernias are more frequent in males than in women and the risk of developing one rises with age.
A hernia can form in children who have a weakening in their abdominal wall or it can be congenital (existing at birth). Hernia can result from activities and medical conditions that put more strain on the abdominal wall. These consist of:
- stooping to use the restroom (maybe due to long-term constipation)
- recurring cough
- Cayman fibrosis
- increased prostate
- effort to urinate
- being obese or overweight
- stomach fluid
- hoisting large objects
- Dialysis in the abdomen
- unsound nutrition
- smoking
- physical effort
- inaccessible testicles
Risk factors for hernia
By kind of hernia, the risk factors can be divided into:
Incisional hernia risk factors
The most obvious risk factor is recent abdominal surgery because an incisional hernia is a result of surgery. Three to six months following the procedure, particularly if:
- They are engaged in demanding work.
- having put on more weight.
- become a mother
All of these elements increase the strain on tissue as it recovers.
Inguinal hernia risk factors
Inguinal hernias are more likely to occur in:
- more likely to develop in those who smoke.
- older people
- people who have experienced inguinal hernias in close relatives
- people with a history of inguinal hernias
- males
- smokers, as tobacco toxins damage tissues and increase the risk of a hernia
- chronic constipation sufferers
- low birth weight and early delivery
- pregnancy
Risk factors for umbilical hernia
Premature babies and infants with low birth weights are more likely to develop umbilical hernias.
- Risk factors for adults include:
- gaining weight
- having several children
- being a woman
Risk factors for hiatal hernia
Hiatal hernia risk is increased in those who:
- are at least 50 years old.
- to be obese
REFERENCES:
- https://www.healthline.com/health/hernia
- https://www.medicalnewstoday.com/articles/142334
- https://my.clevelandclinic.org/health/diseases/15757-hernia
- https://www.webmd.com/digestive-disorders/understanding-hernia-basics
For more details, kindly visit below.